Making the lifestyle changes needed to manage MASLD can be a challenge, but the choices you make today can lead to a healthier tomorrow.
Jump to section
A Bionews and Liver Disease News Special Feature
SCROLL TO ENGAGE
80-100
million
million
people affected
2nd most common
reason for liver transplant
Early
action
action
is key
Metabolic dysfunction-associated steatotic liver disease (MASLD) is the most common chronic liver disease in the U.S., affecting 80-100 million people. Driven by metabolic conditions like obesity, type 2 diabetes, high blood pressure, and high cholesterol, its rising prevalence is a growing public health concern.
More than 2 in 5 adults experience obesity, with rates of 41% among women and 39% among men, making it one of the biggest drivers of MASLD. This condition is often a “silent disease,” meaning symptoms may not appear until significant liver damage has occurred.
In some cases, MASLD progresses to metabolic dysfunction-associated steatohepatitis (MASH), a more severe form that includes liver inflammation and scarring. If left untreated, MASH can lead to fibrosis (scarring), cirrhosis, liver failure, or even liver cancer.
Today, MASLD and MASH are the second most common reasons for liver transplants in the U.S., with related liver cancer being the fastest-growing cause. MASLD is expected to become the leading reason for transplants, highlighting the need for early intervention. Globally, MASLD rates have surpassed 40% in the Americas and Southeast Asia, and cases are projected to rise significantly — affecting 1 in 2 adults — by 2030.
The good news: Progression is not inevitable. Lifestyle changes, such as a balanced diet, regular exercise, and managing diabetes or obesity, can slow or even reverse early-stage MASLD. Cutting processed foods, maintaining a healthy weight, and staying active can improve liver function and reduce complications.
Because MASLD often has no symptoms, early action is key. Understanding risk factors and making informed choices regarding lifestyle can have a lasting impact on liver health. Small but consistent steps can help prevent severe disease and support overall well-being.
In some cases, MASLD progresses to metabolic dysfunction-associated steatohepatitis (MASH), a more severe form that includes liver inflammation and scarring. If left untreated, MASH can lead to fibrosis (scarring), cirrhosis, liver failure, or even liver cancer.
Today, MASLD and MASH are the second most common reasons for liver transplants in the U.S., with related liver cancer being the fastest-growing cause. MASLD is expected to become the leading reason for transplants, highlighting the need for early intervention. Globally, MASLD rates have surpassed 40% in the Americas and Southeast Asia, and cases are projected to rise significantly — affecting 1 in 2 adults — by 2030.
The good news: Progression is not inevitable. Lifestyle changes, such as a balanced diet, regular exercise, and managing diabetes or obesity, can slow or even reverse early-stage MASLD. Cutting processed foods, maintaining a healthy weight, and staying active can improve liver function and reduce complications.
Because MASLD often has no symptoms, early action is key. Understanding risk factors and making informed choices regarding lifestyle can have a lasting impact on liver health. Small but consistent steps can help prevent severe disease and support overall well-being.



MASLD
Explained
Explained
Meet the Patients
Kathryn Hudson
Newspaper editor and reporter Kathryn Hudson's relief from a successful weight-loss surgery didn't last long before she was diagnosed with MASH in 2008.
Stephen W. Smith
As an Army lawyer, Stephen Smith spent decades serving others, but a MASLD diagnosis was a reminder that he needed to focus on his own health.

Walton Harrold
In 2015, IT specialist Walt Harrold faced a wake-up call with his MASLD diagnosis. For the past 10 years, he has been actively managing his health.

MASLD Basics Explained

Watch: Dr. Stine explains the basics of MASLD and how it progresses.
Meet the
Expert
Expert

Our Expert
Jonathan G. Stine, MD
Gastroenterology, Transplant Hepatology
Research Director, Penn State Health Liver Center
An internationally recognized liver expert, Jonathan Stine, MD, is an associate professor at Penn State. He has authored over 115 peer-reviewed papers on MASLD and exercise and leads Penn State’s Fatty Liver Program. An NIH-funded researcher, he was chair of the International Roundtable on MASLD and Physical Activity and serves on hepatology journal editorial boards.
Risk Factors for Progression
- Obesity
- Type 2 diabetes
- High blood pressure
- High triglycerides and low HDL cholesterol
- Genetics
- Other
- Watch video
Risk factor 1
Obesity
Obesity, or having too much body fat, especially around the belly, is one of the biggest risk factors for MASLD. More than 75% of people with MASLD are obese, and in cases of severe obesity, nearly 90% are affected.
Extra fat in the body, especially around the liver or other organs, leads to inflammation and insulin resistance. This causes liver damage to worsen over time. Fat cells also release hormones and chemicals that promote scarring in the liver.
Obesity increases the risk of progressing from fatty liver to advanced liver scarring and cirrhosis. Managing weight through healthy eating and physical activity is one of the best ways to protect the liver and slow disease progression.
Extra fat in the body, especially around the liver or other organs, leads to inflammation and insulin resistance. This causes liver damage to worsen over time. Fat cells also release hormones and chemicals that promote scarring in the liver.
Obesity increases the risk of progressing from fatty liver to advanced liver scarring and cirrhosis. Managing weight through healthy eating and physical activity is one of the best ways to protect the liver and slow disease progression.
Risk factor 2
Type 2 diabetes
People with diabetes have a much higher risk of developing liver disease. Up to 70% of people with MASLD have insulin resistance, meaning their bodies can’t use insulin properly. This leads to high blood sugar and fat buildup in the liver, which can cause scarring.
MASLD is also a pre-diabetic condition, increasing the risk of type 2 diabetes (when the body struggles to regulate blood sugar) by 2 to 5 times, especially with severe liver damage. Because of this, people with type 2 diabetes should be screened for MASLD, regardkess of whether they are experiencing symptoms. Managing blood sugar can help protect the liver.
MASLD is also a pre-diabetic condition, increasing the risk of type 2 diabetes (when the body struggles to regulate blood sugar) by 2 to 5 times, especially with severe liver damage. Because of this, people with type 2 diabetes should be screened for MASLD, regardkess of whether they are experiencing symptoms. Managing blood sugar can help protect the liver.
Risk factor 3
High blood pressure
High blood pressure doesn’t just strain the heart — it also takes a toll on the liver. Elevated blood pressure increases stress on the liver’s small blood vessels, contributing to fibrosis.
Research indicates that MASLD affects approximately 50% of individuals with high blood pressure. Because hypertension often coexists with obesity and diabetes, managing it through medication, a balanced diet, and regular exercise can help protect liver health and reduce long-term damage.
Research indicates that MASLD affects approximately 50% of individuals with high blood pressure. Because hypertension often coexists with obesity and diabetes, managing it through medication, a balanced diet, and regular exercise can help protect liver health and reduce long-term damage.
Risk factor 4
High triglycerides and low HDL cholesterol
High triglycerides and low high-density lipoprotein (HDL) cholesterol, also known as dyslipidemia, are key risk factors for MASLD. Triglycerides (a type of fat in the blood) and HDL (the "good" cholesterol that helps remove fats) are often imbalanced in MASLD patients.
Research shows that elevated lipid levels are common in MASLD. Managing cholesterol through a healthy diet, regular exercise, and medication can help slow liver disease progression and support overall metabolic health.
Research shows that elevated lipid levels are common in MASLD. Managing cholesterol through a healthy diet, regular exercise, and medication can help slow liver disease progression and support overall metabolic health.
Risk factor 5
Genetics
Genetics contribute to MASLD risk by influencing how the liver stores and processes fat. Some people inherit genetic variations that increase their risk of developing MASLD, even if they do not have obesity or diabetes. The PNPLA3 gene variant (I148M) is one of the strongest genetic risk factors, leading to increased liver fat accumulation and a higher likelihood of fibrosis and cirrhosis.
Certain racial and ethnic groups, such as Hispanic populations, have a higher genetic predisposition to MASLD, contributing to its increased prevalence and severity. While genetic predisposition alone does not cause MASLD, it can intensify the effects of metabolic risk factors, making disease progression more likely.
Certain racial and ethnic groups, such as Hispanic populations, have a higher genetic predisposition to MASLD, contributing to its increased prevalence and severity. While genetic predisposition alone does not cause MASLD, it can intensify the effects of metabolic risk factors, making disease progression more likely.
Risk factor 6
Other
MASLD often coexists with conditions that contribute to its progression:
- Polycystic ovary syndrome causes insulin resistance and hormonal imbalances, increasing liver fat.
- Obstructive sleep apnea lowers oxygen and triggers inflammation, worsening liver damage.
- Hypothyroidism slows metabolism, promoting liver fat buildup.
- Growth hormone deficiency increases visceral fat, leading to liver steatosis.
Dr. Stine talks about why regular liver checkups are important for people with any of the MASLD risk factors.
?
QUIZ
Myth or fact?
Your liver plays a crucial role in keeping your body healthy, but there are many misconceptions about liver disease, particularly MASLD and MASH. Do you know the facts from the myths? Take this quick quiz to test your knowledge and learn how lifestyle choices can affect liver health.
Hear More From Our Patients
Stephen, Kathryn, and Walton give some advice for others who have been diagnosed with MASLD, as well as the impact the diagnosis has had on their families.

Kathryn reflects on MASLD warning signs that she'd dismissed before her diagnosis.

Kathryn shares practical tips for how she regulates her diet while still enjoying treats.
Stephen shares his advice on how regular check-ups can make a difference.

Stephen talks about his biggest regret and what he wishes he would have done differently for his health.
Walt shares how living with MASLD affects not only him but his family as well.

Walt talks about how he can’t change the past but he can change his future through healthy choices.
?
This or
That?
Thank You
MASLD progression can be managed. By identifying warning signs and liver disease risks, you can take tangible steps to safeguard your liver health. Small yet steady changes in lifestyle — like proper nutrition, regular exercise, and controlling metabolic conditions — can help slow down or even reverse early damage.
Being aware and taking action is key to making the right choices for your long-term liver health. Whether through early screenings, healthier habits, or medical guidance, preventive measures are one of the best defenses against serious complications later on. Take a step toward better health by caring for your liver.
Being aware and taking action is key to making the right choices for your long-term liver health. Whether through early screenings, healthier habits, or medical guidance, preventive measures are one of the best defenses against serious complications later on. Take a step toward better health by caring for your liver.
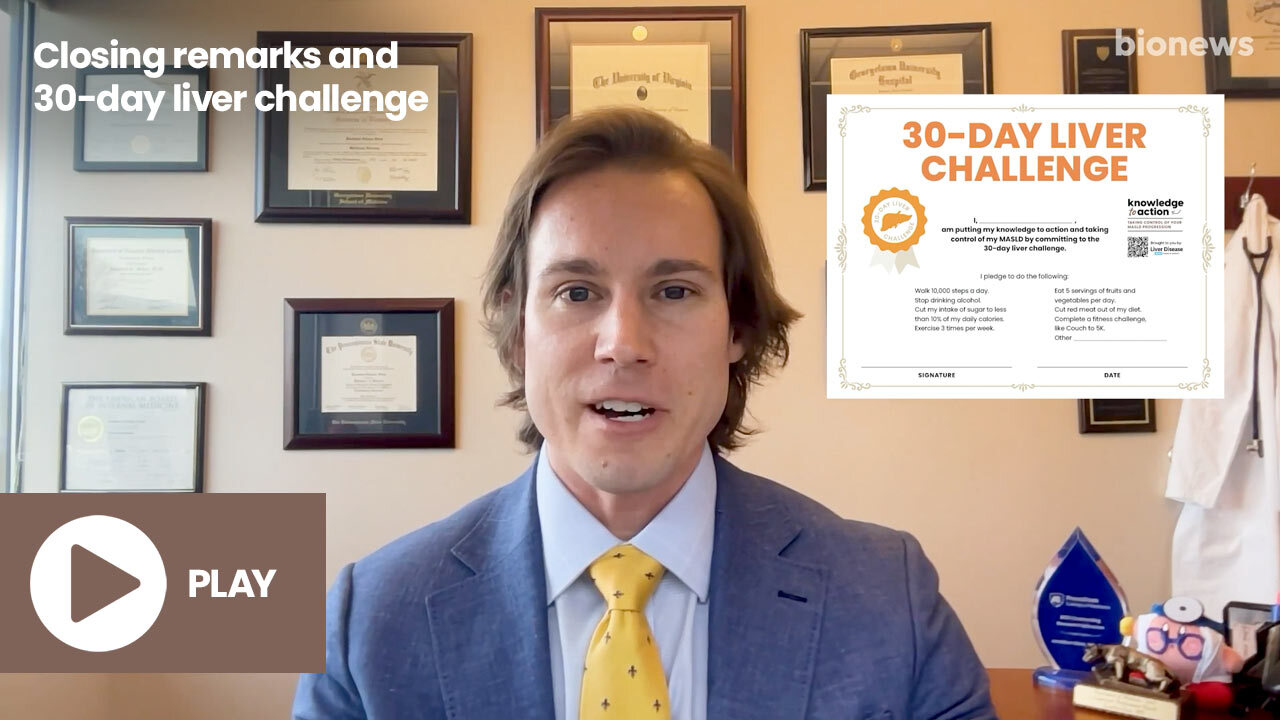
Dr. Stine sums up the importance of getting proactive about your liver health and taking small steps today to lead the life you want to live.
Before you go, take our pledge to prioritize liver health and share your insights in our short survey below.
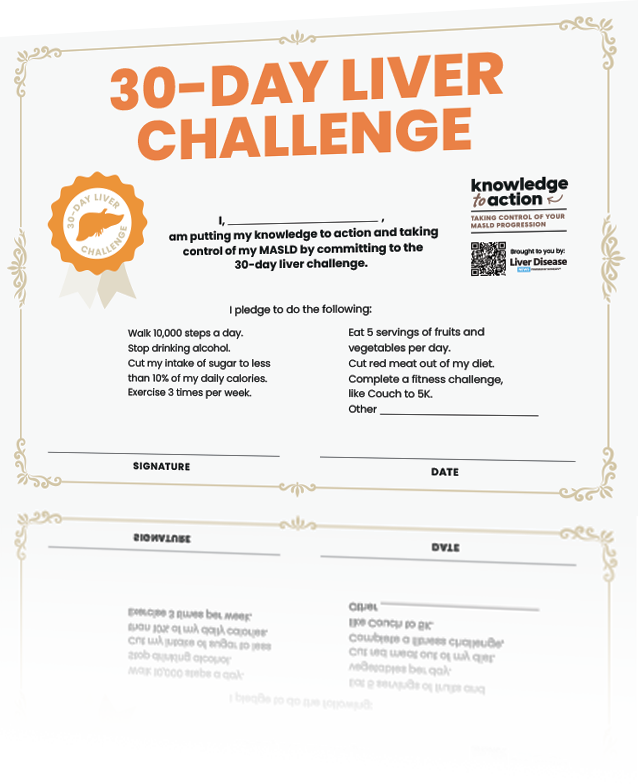
30-Day Liver Challenge
It’s time to put your knowledge to action with our 30-day challenge to better liver health. Take the first step today!
Generate your certificate:
Enter your name and the activities you are pledging to do for 30 days to generate a downloadable certificate that you can print and display.
Let Us Know Your Thoughts
Additional Resources
Discover our Healthy Liver Living guide on Liver Disease News for resources on managing MASLD and MASH.
References
- Ali SMJ, Lai M. Metabolic dysfunction-associated steatotic liver disease. Ann Intern Med. 2025;178(1):ITC1-ITC16. doi:10.7326/ANNALS-24-02933.
- American Liver Foundation. Obesity, MASLD, and MASH fact sheet. Published September 2024. Accessed February 27, 2025. https://liverfoundation.org/wp-content/uploads/2024/09/Obesity.MASLD_.MASH-Fact-Sheet_Final.pdf.
- Parente A, Milana F, Hajibandeh S, et al. MASLD pathophysiology. Dig Liver Dis. 2024;56(3):310-316. doi:10.1016/j.dld.2024.01044-2.
- Le P, Tatar M, Dasarathy S, et al. Metabolic dysfunction-associated steatotic liver disease: recent advances in pathophysiology and clinical management. JAMA Netw Open. 2025;8(1):e32577. doi:10.1001/jamanetworkopen.2025.32577.
- Teng ML, Ng CH, Huang DQ, et al. Global incidence and prevalence of nonalcoholic fatty liver disease. Clin Mol Hepatol. 2023;29(Suppl):S32-S42. doi:10.3350/cmh.2022.0365.
- NHS. Non-alcoholic fatty liver disease. NHS. Accessed February 27, 2025. https://www.nhs.uk/conditions/non-alcoholic-fatty-liver-disease/.
- Vere CC, Streba CT, Streba LM, Ionescu AG, Sima F. Psychosocial stress and liver disease status. World J Gastroenterol. 2009;15(24):2980-2986. doi:10.3748/wjg.15.2980.
- World Health Organization. Alcohol fact sheet. Published June 28, 2024. Accessed February 27, 2025. https://www.who.int/news-room/fact-sheets/detail/alcohol. Marti-Aguado D, Clemente-Sanchez A, Bataller R. Liver disease and metabolic dysfunction: new therapeutic targets. J Hepatol. 2022;77(1):1-14. Available from: https://www.sciencedirect.com/science/article/pii/S0168827822000290.
- Marti-Aguado D, Clemente-Sanchez A, Bataller R. Liver disease and metabolic dysfunction: new therapeutic targets. J Hepatol. 2022;77(1):1-14. Available from: https://www.sciencedirect.com/science/article/pii/S0168827822000290.
- Marti-Aguado D, Clemente-Sanchez A, Bataller R. Advances in the management of metabolic liver disease. Endocr Pract. 2022;28(6):755-761. Available from: https://www.endocrinepractice.org/article/S1530-891X(22)00090-8/fulltext.
- Cleveland Clinic. Nonalcoholic steatohepatitis. Accessed February 27, 2025. https://my.clevelandclinic.org/health/diseases/22988-nonalcoholic-steatohepatitis.
- Gilgenkrantz H, Collin de l'Hortet A. Nonalcoholic fatty liver disease: from pathophysiology to therapy. Am J Pathol. 2018;188(6):1490-1500. Available from: https://www.sciencedirect.com/science/article/pii/S000294401731026X.
- Cleveland Clinic. Fatty liver disease. Accessed February 27, 2025. https://my.clevelandclinic.org/health/diseases>/15831-fatty-liver-disease.
- Francisco V, Sanz MJ, Real JT, et al. Adipokines in non-alcoholic fatty liver disease: Are we on the road toward new biomarkers and therapeutic targets? Biology (Basel). 2022;11(8):1237. doi:10.3390/biology11081237.
- Zheng H, Sechi LA, Navarese EP, Casu G, Vidili G. Metabolic dysfunction-associated steatotic liver disease and cardiovascular risk: a comprehensive review. Cardiovasc Diabetol. 2024;23(1):346. doi:10.1186/s12933-024-02434-5.
- Leith D, Lin YY, Brennan P. Metabolic dysfunction-associated steatotic liver disease and type 2 diabetes: a deadly synergy. touchREV Endocrinol. 2024;20(2):5-9. doi:10.17925/EE.2024.20.2.2.
- Maeda T. The causal relationship between non-alcoholic fatty liver disease, hypertension, and cardiovascular diseases: implications for future research. Hypertens Res. 2024;47(6):2580-2582. doi:10.1038/s41440-024-01759-8.
- Syed-Abdul MM. Lipid metabolism in metabolic-associated steatotic liver disease (MASLD). Metabolites. 2023;14(1):12. doi:10.3390/metabo14010012.
- Walker RW, Belbin GM, Sorokin EP, et al. Genetic architecture of NAFLD and metabolic syndrome traits in diverse populations. J Hepatol. 2020;73(5):1042-1054. doi:10.1016/j.jhep.2020.05.043.
- Shaheen M, Schrode KM, Tedlos M, Pan D, Najjar SM, Friedman TC. Association of metabolic dysfunction-associated steatotic liver disease with physiological and genetic factors. Front Physiol. 2023;14:1076730. doi:10.3389/fphys.2023.1076730.
- WebMD. Fatty liver disease and polycystic ovary syndrome (PCOS). Accessed February 27, 2025. https://www.webmd.com/fatty-liver-disease/fatty-liver-and-pcos.
- Frontiers in Endocrinology. Metabolic dysfunction-associated steatotic liver disease and endocrine factors. Front Endocrinol. 2023;14:1254459. doi:10.3389/fendo.2023.1254459.
- Bikeyeva V, Abdullah A, Radivojevic A, et al. Nonalcoholic fatty liver disease and hypothyroidism: what you need to know. Cureus. 2022;14(8):e28052. doi:10.7759/cureus.28052.
- Bikeyeva V, Abdullah A, Radivojevic A, et al. Nonalcoholic fatty liver disease and hypothyroidism: what you need to know. Cureus. 2022;14(8):e28052. doi:10.7759/cureus.28052.
- Cleveland Clinic. Liver disease. Available from: https://my.clevelandclinic.org/health/diseases/17179-liver-disease. Accessed February 27, 2025.
- American Association for the Study of Liver Diseases (AASLD). New MASLD nomenclature. Accessed February 27, 2025. https://www.aasld.org/new-masld-nomenclature#:~:text=MASLD%2C%20formerly%20known%20as%20NAFLD.
- Mayo Clinic. Pediatric metabolic dysfunction-associated steatotic liver disease (MASLD). Mayo Clinic. Accessed February 27, 2025. https://www.mayoclinic.org/medical-professionals/pediatrics/news/pediatric-metabolic-dysfunction-associated-steatotic-liver-disease-masld.
- Komolafe O, Buzzetti E, Linden A, et al. Nutritional supplementation for nonalcohol-related fatty liver disease: a network meta-analysis. Cochrane Database Syst Rev. 2021;7(7):CD013157. doi:10.1002/14651858.CD013157.pub2.
- Mayo Clinic. Dietary fats: know which types to choose. Accessed February 27, 2025. https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/fat/art-20045550.
- Mayo Clinic. Mayo Clinic Minute: Is a fruit smoothie a good meal replacement option? Accessed February 27, 2025. https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-minute-is-a-fruit-smoothie-a-good-meal-replacement-option/.
- Healthline. Are granola bars healthy? Accessed February 27, 2025. https://www.healthline.com/nutrition/are-granola-bars-healthy.
- Vell MS, Creasy KT, Scorletti E, et al. Omega-3 intake is associated with liver disease protection. Front Public Health. 2023;11:1192099. doi:10.3389/fpubh.2023.1192099.
- Cleveland Clinic. Is coffee good for your liver? Published January 29, 2025. Accessed February 27, 2025. https://health.clevelandclinic.org/is-coffee-good-for-your-liver.
- Bellar A, Welch N, Dasarathy S. Exercise and physical activity in cirrhosis: opportunities or perils. J Appl Physiol. 2020;128(6):1547-1567. doi:10.1152/japplphysiol.00798.2019.