CNP-104 shown to safely reduce liver scarring in PBC Phase 2 trial
Therapy could be first disease-modifying treatment for PBC: Developer
Written by |
Two infusions of the investigational therapy CNP-104 safely reduced liver scarring (fibrosis) and led to beneficial changes in disease-related immune cell populations among adults with primary biliary cholangitis (PBC).
That’s according to four-month top-line data from an ongoing proof-of-concept Phase 2a clinical trial (NCT05104853), in which participants are being followed for up to two years.
Should further clinical studies find CNP-104 beneficial in PBC, the treatment could be the first to directly address the underlying autoimmune cause of the rare liver condition, according to developer Cour Pharmaceuticals.
“These data highlight the potential of CNP-104 to be the first disease-modifying treatment for people living with PBC,” Paul M. Peloso, MD, Cour’s chief medical officer, said in a company press release. “We look forward to presenting these encouraging data at an upcoming scientific meeting.”
First-line treatments for PBC only ease disease symptoms
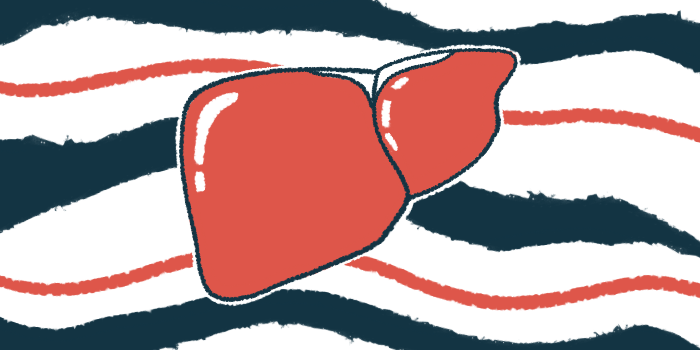
PBC, a rare liver disease affecting mainly women, is characterized by chronic cholangitis, or inflammation in the series of ducts that carry the digestive fluid bile out of the liver and to the intestines. It’s believed to be caused by an underlying autoimmune disease in which the body’s immune system mistakenly launches an inflammatory attack against its own healthy tissue.
In the long-term, bile duct inflammation can result in stalled bile flow — a condition known as cholestasis — that makes bile accumulate to toxic levels in the liver, ultimately leading to scarring, known as fibrosis, and serious liver damage.
The first-line treatment for PBC is ursodeoxycholic acid (UDCA), sold as Urso and Actigall, with generics available, which helps to increase bile flow. Other therapies, including Ocaliva (obeticholic acid), Iqirvo (elafibranor), and Livdelzi (seladelpar) can be used as second-line treatments if UDCA is ineffective or poorly tolerated.
But while these therapies can help ease the symptoms of PBC, they don’t directly address its underlying autoimmune cause.
“Despite the recent evolution of the PBC treatment landscape, there remains a significant unmet need for new treatments,” said Christopher Bowlus, MD, the trial’s principal investigator and the Lena Valente professor and chief of the gastroenterology and hepatology division at the University of California, Davis.
CNP-104 intends to address the underlying cause of PBC by helping the immune system learn how to tolerate, or recognize and leave alone, the healthy parts of the body that it wrongfully attacks in PBC.
About 95% of all PBC patients have self-reactive antibodies called anti-mitochondrial antibodies (AMAs), which mainly target the E2 component of a complex of three mitochondrial enzymes collectively called the pyruvate dehydrogenase complex (PDC). Mitochondria are the powerhouses of cells and provide energy.
Based on Cour’s nanoparticle platform, CNP-104 is comprised of biodegradable nanoparticles containing the PDC-E2 component. These nanoparticles are taken up by certain immune cells and released in the liver and spleen upon their death.
This ultimately results in the presentation of PDC-E2 to immune T-cells in the absence of inflammatory signals, making the cells perceive the molecule as self and suppressing subsequent immune responses against PDC-E2.
As such, the therapy is expected to train immune T-cells, which are drivers of the autoimmune attacks, to tolerate PDC-E2, thereby easing inflammation and preventing liver damage.
CNP-104 found to reduce liver stiffness, a marker of scarring
The ongoing, U.S.-based Phase 2a trial is evaluating CNP-104’s safety, tolerability, pharmacological properties, and efficacy against a placebo. It involves 41 adults with PBC, ages 18-75, who were unresponsive to treatment with UDCA and/or Ocaliva.
The participants were randomly assigned to receive either one of two doses of CNP-104 (4 or 8 mg/kg) or a placebo, one week apart, on days 1 and 8, via an infusion directly into the bloodstream (intravenously).
Top-line data concerned the study’s primary period of 120 days, or about four months. Meanwhile, participants are continuing to be monitored in a 20-month, or slightly longer than 1.5-year, safety evaluation.
These results showed a statistically significant reduction in liver stiffness, a marker of liver fibrosis as assessed with Fibroscan, among patients treated with CNP-104 compared with those on the placebo.
“These data suggest that CNP-104 has the potential to halt disease progression which would be a transformational advancement for people living with PBC,” Peloso said.
Those given the placebo tended to experience a greater decrease in blood levels of albumin compared with those given CNP-104. Low blood albumin levels are an indicator of liver damage.
Moreover, treatment with CNP-104 was associated with favorable changes in disease-driving CD4 T-cells and tolerance-inducing CD8 T-cells, indicating the therapy was working as intended to create immune tolerance.
These data suggest that CNP-104 has the potential to halt disease progression which would be a transformational advancement for people living with PBC.
CNP-104 treatment also was associated with significantly higher rates of an immune response concerning a reduction in both number and proportion of a type of pro-inflammatory T-cells called Th17 cells.
The therapy was generally safe and well tolerated, with all treatment-related adverse events being reported as mild in severity.
According to Bowlus, “While these data are early and from a small number of patients, they are incredibly promising and merit future investigation.”
CNP-104 has been granted fast track designation in the U.S. for treating PBC. That status is meant to accelerate a therapy’s clinical development and regulatory review.