Less invasive Kasai surgery works better for infants with BA: Study
Less blood loss with laparoscopy, though long-term outcomes were comparable
Written by |
Using a minimally invasive method called laparoscopy to conduct standard Kasai surgery significantly reduces blood loss and increases the chances of jaundice clearance compared with traditional open surgery in infants with biliary atresia (BA), a new study reports.
Kasai surgery is a procedure designed to restore the flow of the digestive fluid bile, which normally moves from the liver to the intestines, that’s often used for babies with the rare liver disease. Jaundice, a common biliary atresia symptom, refers to the yellowing of the skin and white parts of the eyes that results from bile accumulation into the bloodstream.
Still, the researchers noted that long-term outcomes, such as survival, were comparable with either approach. Surgery time is longer with the less invasive method, the data showed.
Additionally, the study demonstrated that infants who did not respond to surgery received higher doses of prednisolone, an anti-inflammatory and immunosuppressive medication, relative to those who did. This approach, however, was not associated with better outcomes, and actually was linked to a greater chance of needing a liver transplant, according to the team.
Overall, the findings suggest that “laparoscopic [Kasai procedure] can be the first-line treatment for BA, and excessive steroid administration to extend NLS [native liver survival] should be discontinued,” the researchers stated as an “implication” of their work.
The study, “Impact of laparoscopic Kasai portoenterostomy on long-term native liver survival in patients with biliary atresia: a multicentre propensity score-matched study,” was published in the journal Hepatobiliary Surgery and Nutrition.
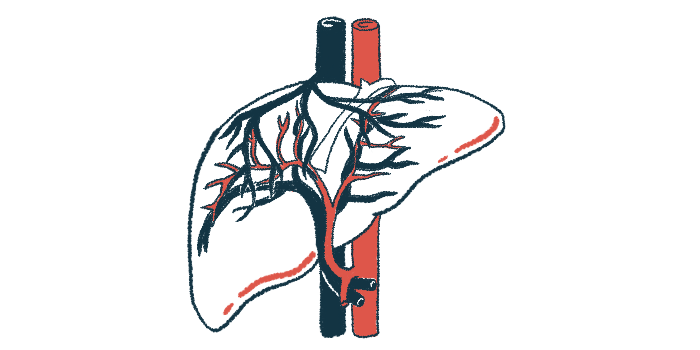
Bile is a digestive fluid that’s produced in the liver and then shipped out to the intestines through a series of tubes called bile ducts.
BA is a congenital disorder in which the bile ducts are absent or blocked off, so bile cannot flow out of the liver properly. As a consequence, the fluid builds up in the liver, which can cause liver damage, leading to symptoms such as jaundice.
The first-line treatment is the Kasai procedure, an operation that aims to create a new channel through which bile can flow out of the liver to the intestines. Still, over the long run, children with BA will often develop worsened liver disease, and a liver transplant may become the only therapeutic option.
Comparing outcomes of new vs. traditional approach to Kasai surgery
Traditionally, the Kasai surgery is done by making a large incision in the abdomen to give surgeons access to the liver.
A newer approach is to use laparoscopy, where tiny cameras are inserted into the body through small incisions, and surgeons use these cameras and associated tools to perform the procedure without opening up the abdomen.
The newer technique is becoming more common. “However, the role of laparoscopy in mid- and long-term NLS outcomes remains unclear,” the researchers wrote.
In addition, while some studies have reported benefits with steroid therapy — a class of medications that includes prednisolone — others found no improvements in NLS, meaning that it does not delay the time of liver transplant.
To address these uncertainties, a team of scientists in Japan assessed outcomes from 356 infants with BA who underwent the Kasai procedure using either standard techniques or laparoscopy at centers in Asian nation between 2000 and 2022.
The children underwent surgery at a median of 62 days of age, or about 2 months, and were followed for a median of 13 years.
Using less invasive technique resolved jaundice in over 80% of infants
Using a statistical tool called propensity score matching to account for presurgery differences between the groups, the scientists calculated whether there were any meaningful differences in outcomes between the two approaches.
The results showed that the number of infants who died or needed a liver transplant in the five years following surgery — long-term outcomes — was comparable with both approaches. However, the number of infants whose jaundice resolved as a short-term outcome was significantly higher (81% vs. 64%) among those for whom the less invasive strategy was used.
“Laparoscopy showed a significantly higher jaundice clearance rate than the open approach in all cases,” the researchers wrote.
The less invasive procedure usually took about an hour longer to perform, but it was associated with a 68% significant reduction in blood loss, according to the researchers. Rates of surgical complications were comparable between the two groups.
Laparoscopy showed a significantly higher jaundice clearance rate than the open approach in all cases. … Considering the [outcomes] … laparoscopic [Kasai surgery] can be a standard treatment option for biliary atresia.
The data led the researchers to suggest that, “considering the [survival and liver transplant outcomes] and severe complications rate in the laparoscopic KPE [Kasai surgery] was comparable to the open KPE, laparoscopic KPE can be a standard treatment option for BA.”
The team also noted that, following Kasai surgery, infants who did not experience jaundice clearance were given significantly higher doses of prednisolone compared with those who did.
Further statistical analyses showed that the children given prednisolone doses above the median (90 mg/kg) were significantly more likely, by 70%, to undergo a liver transplant — implying that increasing prednisolone dosage beyond a certain point may not be beneficial.
Yoichi Nakagawa, MD, a study coauthor at Nagoya University, said in a university press release that “steroid therapy is commonly used as postoperative care in many pediatric centers worldwide to reduce inflammation and help the liver produce bile.” He noted, however, that “protocols vary significantly between institutions.”
Steroid use should be studied further, according to the researcher.
“Our findings suggest that while steroid therapy itself may provide certain benefits, increasing the dose beyond a certain point does not necessarily improve outcomes,” Nakagawa said.