Alagille syndrome diagnosis
Last updated Jan. 20, 2025, by Lindsey Shapiro, PhD

Reaching a diagnosis of Alagille syndrome, a rare genetic disease that causes problems in the liver and other organs, can be difficult because the symptoms vary widely for every person.
Doctors may make a diagnosis by identifying characteristic signs of the disease and ruling out other more common conditions in a series of Alagille syndrome tests, including physical and eye exams, blood tests, imaging scans, and liver biopsy. Genetic testing to look for disease-causing mutations can confirm the diagnosis in most patients.
Alagille is most commonly caused by mutations in the JAG1 or NOTCH2 genes, which are important for embryonic development. Consequently, people with Alagille syndrome exhibit a range of developmental abnormalities, including liver problems, heart or kidney issues, characteristic facial features, and blood vessel and bone abnormalities that are usually evident in infancy or childhood.
Although reaching an Alagille syndrome diagnosis can be challenging, identifying the disease early and accurately is critical. This will ensure that patients receive proper care and treatment as soon as possible, which can ease symptoms and help avoid or delay life-threatening complications.
The importance of early diagnosis
Left untreated, the liver problems and heart defects that affect most Alagille patients can be life-threatening. Patients may also have blood vessel abnormalities in the neck and brain, which can increase the risk of stroke.
Currently, there isn’t a cure for Alagille, but there are several therapeutic approaches, including medications and surgeries, that can lessen the burden of symptoms and make it easier to live with the disease. Certain interventions, such as liver or heart surgery, can also help to minimize, delay, or prevent more serious and potentially fatal problems with these organs later on, including liver failure, which may require a liver transplant.
Recognizing the early signs of Alagille and reaching out to a doctor as soon as possible is therefore a key first step for ensuring that the rare liver disease is properly diagnosed and managed.
Symptoms to look out for
Alagille can affect a range of body systems, most commonly leading to problems with the liver, heart, and eyes, as well as facial changes. While the symptoms of Alagille syndrome can vary from person to person, nearly all patients experience liver problems.
Most often, this is characterized by problems with the bile ducts, the series of tubes that carry the digestive fluid bile from the liver to the small intestine. Bile not only helps to break down and absorb fatty molecules in the intestines, but is also needed to carry certain waste products into the intestines to be excreted in feces. People with Alagille tend to have fewer than normal bile ducts in their liver, which causes bile flow to be stalled — a condition called cholestasis — and its components to toxically accumulate in the liver and bloodstream.
The earliest noticeable signs of Alagille — typically evident in infancy or childhood — are usually related to problems with the liver and bile flow. These may include:
- jaundice, or a yellowish discoloration of the skin and whites of the eyes
- loose, greasy, and pale-colored stools
- dark urine
- poor growth or weight gain
- itchy skin, or pruritus
- xanthomas, or fatty deposits under the skin that appear waxy and yellowish.
Characteristic facial features, including a broad forehead, deeply set and widely spaced eyes, a pointed chin, and a straight nose with a bulbous tip, may also be noticeable in children with Alagille syndrome. However, these might not be easy to detect in infancy and might not be noticed until later in childhood.
If parents or caregivers notice any possible signs of Alagille in their child, they should reach out to a medical professional who can run more tests to establish a diagnosis. Other common Alagille-related problems — such as heart defects and eye problems — as well as less common symptoms affecting the bones, kidneys, and blood vessels, might be detected only through specialized medical tests, so it’s important to seek input from a doctor as soon as possible.
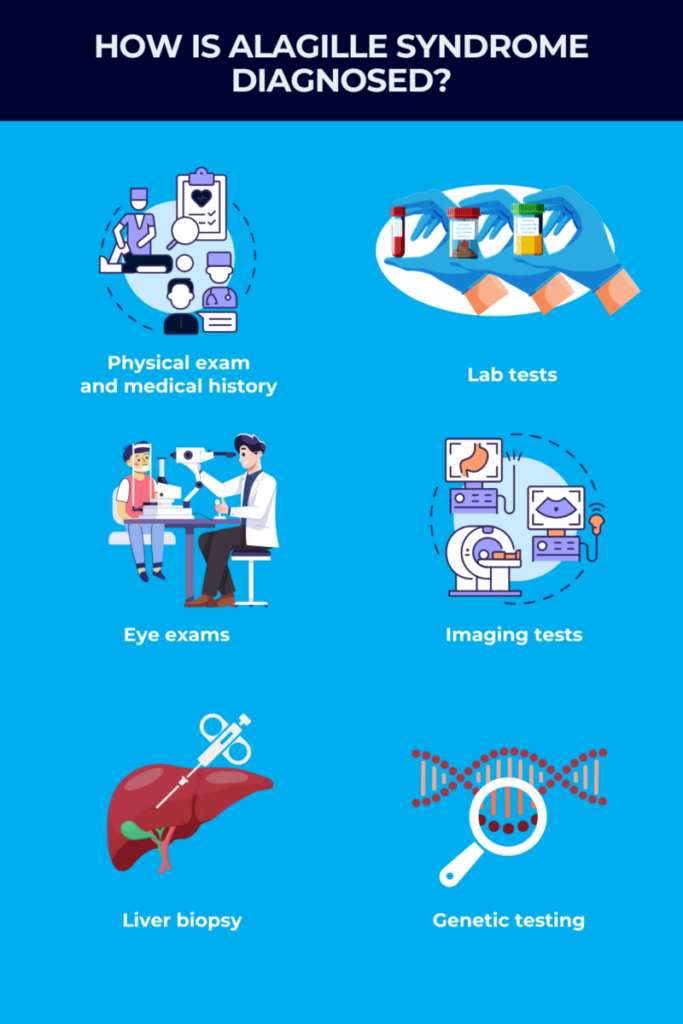
Diagnosing Alagille syndrome
The process of diagnosing Alagille syndrome usually starts with a doctor collecting a detailed medical history. They’ll want to know about any noticeable symptoms and their duration, and whether there’s a family history of Alagille or other liver conditions. A healthcare provider will also perform a thorough physical exam to look for signs and symptoms of the disease, such as:
- jaundice
- scratch marks on the skin from pruritus
- xanthomas
- an enlarged liver or spleen
- characteristic facial features
- heart murmurs, an extra or unusual sound heard during a heartbeat due to the abnormal flow of blood through the heart.
If a physician suspects Alagille, they will likely order a series of other medical tests, including lab and imaging studies, that can help rule out other conditions and confirm the diagnosis.
A diagnosis of Alagille syndrome is generally confirmed when a person has at least three of the seven major signs and symptoms of the disease:
- liver problems usually marked by cholestasis, pruritus, and/or xanthomas
- heart defects, such as peripheral pulmonary stenosis, or the narrowing of the blood vessels that carry blood from the heart to the lungs
- distinctive facial features
- eye abnormalities, such as posterior embryotoxon, which is characterized by a white ring lining the clear transparent layer covering the eyeballs
- bone abnormalities, including butterfly vertebrae, or an irregular, butterfly-like shape of the bones that make up the spine
- kidney defects, such as underdeveloped kidneys
- blood vessel abnormalities, including narrowing or bulging of vessels in the neck, brain, liver, and kidneys.
In cases where there’s a family history of Alagille or where genetic testing confirms the presence of a disease-causing mutation, fewer clinical features are generally required to establish an Alagille syndrome diagnosis.
If a person has symptoms suggestive of Alagille, a doctor will likely order a number of diagnostic tests, which may include:
- lab tests
- eye exams
- imaging tests
- more invasive procedures like a liver biopsy
- genetic testing.
Laboratory testing
A healthcare provider may order blood, stool, or urine tests to look for Alagille-related problems or rule out other diseases that may have similar symptoms. Some things that might be checked for in Alagille tests include:
- blood levels of liver enzymes, including alkaline phosphatase and gamma-glutamyl transpeptidase, which are usually higher than normal in people with Alagille
- blood levels of bilirubin, a waste product that’s normally incorporated into bile to be excreted through feces, but backs up into the bloodstream with Alagille-related cholestasis
- blood clotting, as many clotting players are produced by the liver or absorbed in the intestines through the action of bile
- blood levels of bile acids, the main component of bile, which may spill into the bloodstream and be higher than normal in Alagille patients
- levels of cholesterol or other fats in the blood, which may be increased in people with Alagille
- blood levels of fat-soluble vitamins, such as vitamins A, D, E, and K, which are often reduced in Alagille
- fat levels in the stool, which can be increased due to poor absorption of dietary fats in the intestine
- blood and urine markers of kidney function, which may be impaired in Alagille.
Ophthalmological exam
Most Alagille patients have eye abnormalities, with the hallmark one being posterior embryotoxon. Another common eye manifestation is optic disk drusen, where fatty proteins and calcium deposit in the back region of the eye. Both of these eye symptoms are very common in Alagille but occur only in a minority of people from the general population, so detecting them can aid in reaching an Alagille diagnosis.
Posterior embryotoxon, optic disk drusen, and certain other eye issues may not cause overt vision problems and can only be detected via specialized tests run by an ophthalmologist during an eye, or ophthalmologic, exam.
In addition to standard vision tests, a doctor may perform a slit-lamp test, where a microscope with a bright light is used to visualize all parts of the eye in detail. This allows them to detect posterior embryotoxon or other abnormalities that may point toward a possible Alagille diagnosis.
Imaging studies and more invasive procedures
A variety of different imaging tests might be used to look for physical problems related to Alagille syndrome or to rule out other conditions.
Because liver and biliary problems are a hallmark of the disease, doctors may run several types of imaging to identify problems in these areas.
- An abdominal ultrasound, which uses high-frequency sound waves to create pictures of internal organs, can visualize structural abnormalities in the liver and bile ducts.
- Magnetic resonance cholangiopancreatography, or MCRP, is a type of MRI scan that uses a dye to better visualize the bile ducts and related organs.
- A hepatobiliary iminodiacetic acid, or HIDA, scan involves injecting a radioactive tracer into the bloodstream that will be taken up by bile-producing liver cells. The movement of bile through the biliary system can then be visualized with a specialized scanner. If it doesn’t move as expected, it’s a sign of cholestasis.
All of the above imaging tests are noninvasive ways to look for liver and bile duct abnormalities and to determine their cause. Depending on what’s found in these exams, a more invasive test called an endoscopic retrograde cholangiopancreatography (ERCP) might also be used to provide more detailed information about any liver and bile duct problems.
ERCP is a surgical procedure that’s done under anesthesia. A long, thin tube with a camera attached, called an endoscope, is inserted through the mouth and down into the small intestine. Once in place, a dye is injected through the endoscope into the bile ducts, which allows doctors to visualize these duct systems on an X-ray and detect any problems.
During the ERCP procedure, doctors can also collect a tissue biopsy and treat certain problems in the ducts, like removing blockages or placing tubes to widen narrowed ducts.
Beyond the liver and bile ducts, other imaging tests might also be run to look for clinical features of Alagille, including:
- ultrasound to identify kidney issues
- echocardiogram, a specialized type of ultrasound that can identify heart disease
- X-rays to look for characteristic skeletal abnormalities, including butterfly vertebrae or other problems with the bones of the spinal column
- magnetic resonance angiography, a specialized type of MRI scan to check for blood vessel abnormalities.
If results from noninvasive and minimally invasive procedures don’t confirm or rule out Alagille syndrome, doctors may order a liver biopsy, where a small sample of tissue is removed and sent to the lab for analysis.
A liver biopsy can identify bile duct paucity — where the number of bile ducts in the liver is reduced — which is a core feature of Alagille. However, bile duct paucity will not always be evident in very young infants with Alagille, requiring additional tests. The features observed on a liver biopsy might also help doctors rule out other conditions that can cause liver and bile duct issues.
Genetic testing
Nearly 95% of Alagille cases are caused by mutations in the JAG1 gene, and around 2.5% arise from NOTCH2 gene mutations. As such, genetic testing to identify these mutations can be used to establish an Alagille diagnosis for the vast majority of patients.
To perform genetic testing, doctors collect a small blood sample and send it for analysis in a special lab. If a genetic change associated with Alagille is identified and considered likely to be causing a person’s symptoms, an Alagille syndrome diagnosis can be confirmed. In that case, it may also be recommended that other family members are tested.
There are a couple different approaches to genetic testing that might be taken, depending on the situation. Often, a doctor will start by specifically screening for mutations in JAG1 or NOTCH2 if they suspect the disease, as those are the most likely causes of Alagille. In instances where the clinical picture is less certain, or if individual gene tests are negative, a multigene panel may be run to look for mutations in JAG1 and NOTCH2, as well as other genes that could be causing similar symptoms.
This can also help to rule out other genetic causes of a person’s symptoms. If a doctor suspects a genetic condition, but hasn’t honed in on Alagille as a possibility, more comprehensive genetic testing to screen all the genes in the body might be performed.
A small proportion of Alagille patients do not have identifiable mutations in JAG1 or NOTCH2. For these individuals, a diagnosis will rely on clinical findings from other tests, including the physical exam, lab tests, imaging studies, and liver biopsy.
Differential diagnosis of Alagille syndrome
Identifying Alagille can be complicated by the fact that there are a number of other conditions with overlapping symptoms, and doctors will need to exclude those before confirming an Alagille syndrome diagnosis.
Biliary atresia is a rare disease that can present with very similar symptoms to Alagille in infancy, including those related to cholestasis, as well as defects in the heart and kidneys. Moreover, while biliary atresia is not generally considered an inherited condition, JAG1 mutations have been identified in a subset of patients. Biliary atresia is the most common cause of cholestasis in infants, which may prompt doctors to suspect it before they consider Alagille.
Still, certain features of Alagille, such as the characteristic facial features and eye abnormalities, don’t usually occur in biliary atresia. Findings from imaging and liver biopsy studies can also help distinguish the two disorders.
Other conditions that may be considered in the differential diagnosis of Alagille include:
- neonatal hepatitis
- progressive familial intrahepatic cholestasis
- DiGeorge syndrome
- alpha-1 antitrypsin deficiency
- cystic fibrosis.
Most of these conditions have clinical features that can be distinguished from Alagille syndrome through a careful examination and certain medical tests. If a child is suspected to have Alagille or another liver disease, referral to specialists, such as hepatologists (liver specialists), with experience in diagnosing these conditions may help to reach an accurate diagnosis early on.
Challenges in diagnosing Alagille syndrome
In addition to ruling out other diseases with overlapping symptoms, there are a number of other challenges in diagnosing Alagille.
There’s no one clinical picture that describes every person with Alagille — its symptoms and their severity can be highly variable, even within members of the same family — making it harder for doctors to pinpoint a diagnosis. For example, while the vast majority of patients have bile duct paucity and cholestasis, a minority may not. Other features, like skeletal abnormalities or kidney problems, will occur in some patients but not in others.
Moreover, while Alagille often presents in infancy or childhood, symptoms in mild cases may not be apparent until significantly later in life, leading to a late diagnosis.
Identifying Alagille-causing mutations is therefore a key part of obtaining an accurate diagnosis. Still, the advanced imaging and genetic technology that may be required may not be readily accessible in all regions, making Alagille more difficult to diagnose.
Pediatricians and other primary care providers might not be familiar with how to diagnose Alagille syndrome or how to recognize the signs of the rare disease. In the presence of signs or symptoms suggestive of Alagille, it’s important to seek input from a multidisciplinary team of specialists, including hepatologists, cardiologists, ophthalmologists, geneticists, and others, who can help pinpoint the diagnosis and rule out other possible causes of a person’s symptoms.
Once Alagille is diagnosed, these specialists will also help to design an appropriate management plan for treating the body-wide disease.
Liver Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- New animated video aims to support children living with biliary atresia
- New immune therapy for chronic hepatitis B slashes virus levels in trial
- Skipping PBC treatment leads to longer hospital stays, higher costs: Study
- Distinguishing between PFIC3, Wilson’s disease key for optimal outcomes
- The different ways fatty liver disease affects women vs. men
Related content