Cholangitis diagnosis
Last updated Jan. 17, 2025, by Lindsey Shapiro, PhD

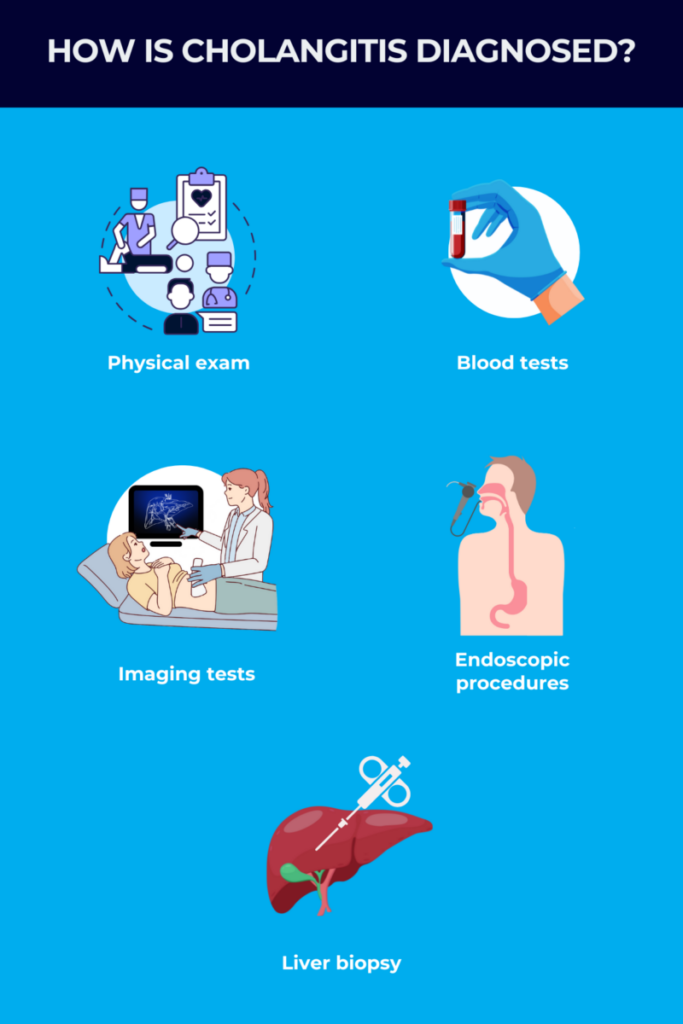
Cholangitis, a condition marked by inflammation in the tubes that carry the digestive fluid bile from the liver into the small intestine, is diagnosed through a series of medical tests, including a physical exam, blood tests, and imaging studies.
The most common cause of cholangitis is a bacterial infection in the bile ducts. These infections are usually related to a blockage somewhere in the biliary system, often due to gallstones (hardened deposits of bile) that obstruct the common bile duct which carries bile to the intestines.
Other possible causes of cholangitis include tumors, parasites, or autoimmune diseases. As the therapeutic approach used in each of these different situations can vary, an important part of diagnosing cholangitis involves identifying what is causing it.
Cholangitis can ultimately cause the flow of bile to be slowed or stalled — a condition called cholestasis — and result in life-threatening consequences if not treated promptly. These consequences may include whole-body infections, irreversible liver damage, or the need for liver transplantation.
Reaching an accurate cholangitis diagnosis as early as possible is essential for patients to promptly receive adequate treatments that can avoid or delay the disease’s more serious complications.
The importance of early diagnosis
Acute forms of cholangitis, including those caused by infections or bile duct blockages, develop suddenly and can rapidly lead to life-threatening complications such as liver failure and sepsis, a severe immune response to infection that causes organs to shut down.
Chronic forms of cholangitis, such as primary biliary cholangitis (PBC), primary sclerosing cholangitis (PSC), and secondary sclerosing cholangitis, come on more slowly, but can cause irreversible liver damage and liver failure in the long term.
In either case, it’s important for patients to speak with a healthcare provider as soon as they experience any signs or symptoms that might be indicative of cholangitis, even if they seem subtle. This will allow doctors to diagnose the condition and identify its underlying cause as early as possible, enabling it to be treated before these more serious complications arise.
Cholangitis symptoms to look out for
Symptoms of cholangitis can vary based on its underlying cause, but some common ones include:
- pain on the upper right side of the abdomen, where the bile duct system is located
- fever and chills
- jaundice, or a yellowish discoloration of the skin and whites of the eyes
- itchy skin, or pruritus
- nausea and vomiting
- dark urine
- pale stools
- fatigue.
Acute cholangitis, also known as ascending cholangitis, typically appears as a trio of symptoms — abdominal pain, fever, and jaundice — that are together known as Charcot’s triad. This triad of symptoms may also come alongside altered mental state and signs of sepsis (including fast heart rate and low blood pressure), a combination known as the Reynold’s pentad.
These symptoms usually come on quickly and are very noticeable. However, many patients may not have these classic symptoms, which can make it harder to diagnose.
In turn, symptoms of chronic cholangitis may not be noticeable until substantial liver damage has occurred, but some of the earliest symptoms may include fatigue, pruritus, and abdominal pain.
Diagnosing cholangitis
If cholangitis is suspected based on a person’s symptoms, several different cholangitis tests might be performed to rule out other possible causes and confirm the diagnosis. This usually starts with an initial evaluation, during which a doctor will review a person’s medical history and perform a physical exam.
When collecting a medical history, a doctor will want to know which symptoms the person has been experiencing and for how long. They’ll also ask questions to assess the presence of any potential risk factors for cholangitis, such as a history of gallstones or certain infections, recent surgery to the bile ducts and nearby tissues, or a family history of certain autoimmune diseases.
During a physical exam, doctors will look for signs of cholangitis, including:
- abdominal pain and tenderness
- an enlarged liver or spleen
- fever
- jaundice
- low blood pressure or fast heart rate
- changes in mental status.
If a person has symptoms of cholangitis, a doctor will likely order a number of diagnostic tests, which may include:
- blood tests
- imaging tests
- endoscopic exams to look inside the body with a camera
- liver biopsy.
Blood tests
Healthcare providers may initially order blood tests to look for signs of inflammation, infection, or liver damage that may be indicative of cholangitis.
- A complete blood count can tell doctors if there is a higher-than-usual number of white blood cells, or immune cells, which can indicate an infection.
- Liver function tests evaluate if the liver is working properly. Elevations in the levels of certain liver enzymes, including alkaline phosphatase and gamma-glutamyl transpeptidase, and bilirubin, a yellow-reddish waste product that’s normally incorporated into bile to be excreted through feces, are commonly seen in cholangitis.
- Blood cultures can be run to look for microbes in the blood that can cause cholangitis, including the bacteria Escherichia coli and Klebsiella.
- Tests for self-reactive antibodies associated with PBC can help diagnose the autoimmune disease. These specific self-reactive antibodies are present in nearly all people with PBC, but rarely found in healthy people.
Doctors may also run several other blood tests to check a person’s general health condition and rule out other possible causes of their symptoms.
Imaging studies
If cholangitis is suspected, imaging tests will usually be performed to visualize the liver and bile duct system and identify any blockages or areas of damage. Imaging tests can also be used to rule out other possible issues that may explain a person’s symptoms.
Noninvasive imaging tests that may be employed to diagnose cholangitis include:
- abdominal ultrasound
- CT scan
- magnetic resonance cholangiopancreatography, or MRCP.
An abdominal ultrasound, which uses high frequency sound waves to create images of the internal organs, is often the first-line imaging test to look for problems in the bile ducts or gallbladder, where bile is stored before being transported to the small intestine.
If a person has acute cholangitis, ultrasound findings may include the thickening of bile duct walls, widening of the bile ducts, or the presence of pus that is commonly the result of bacterial infections. An ultrasound can also detect gallstones or other things that may be obstructing bile flow.
CT scans might also be performed to help better visualize problems such as tumors, abscesses (pus-filled areas), and inflammation in the liver, bile ducts, and nearby tissues. These scans can help rule out other conditions with overlapping symptoms.
MRCP is a specialized type of MRI scan that can determine the location and cause of bile duct obstructions, and may be used when results from ultrasound or CT scans are inconclusive. With this test, a contrast dye is infused into the bloodstream to enable doctors to better visualize the abdominal organs and bile ducts.
This procedure can identify things like bile duct cancer, gallstones, narrowed or dilated bile ducts, and inflammation in the gallbladder or the pancreas (a nearby gland that produces enzymes needed for digestion). MRCP is the test of choice for confirming a PSC diagnosis, with characteristic findings being areas of bile duct narrowing, or strictures, and bile duct widening.
Endoscopic and invasive procedures
When noninvasive diagnostic tests lead to a high suspicion of cholangitis, other tests have been inconclusive, or a person is not able to undergo an MRI scan, a more invasive procedure called endoscopic retrograde cholangiopancreatography, or ERCP, can be used to confirm a cholangitis diagnosis.
While an ERCP looks for the same problems as an MRCP, it’s a more invasive procedure that requires anesthesia. During an ERCP, a long flexible tube with a camera attached, called an endoscope, is inserted through the mouth and down into the small intestine. A dye is injected through the endoscope into the bile ducts, and its movement through the bile ducts can be visualized on an X-ray, allowing the detection of possible blockages.
In addition to visualizing the bile ducts and related structures, an ERCP can also be used to perform biliary drainage procedures if a blockage is found. These procedures may include:
- breaking up and removing gallstones
- removing tumors or collecting samples for analysis
- stretching narrowed bile ducts or placing a small expandable tube, called a stent, to help keep them open
- repairing leaky or injured bile ducts.
Tissue samples collected from bile ducts during ERCP and sent to the lab for analysis can tell doctors more about the extent of damage and inflammation, and help them rule out other diagnoses when imaging tests haven’t been conclusive.
Another minimally invasive scan-guided procedure that may be used to reach a cholangitis diagnosis and also to drain a blocked bile duct is percutaneous transhepatic cholangiography (PTC). Here, a thin needle is inserted through the abdomen into the liver, to inject a special dye into the bile ducts. The dye lets a doctor see the bile ducts on an X-ray. Similarly to ERCP, PTC may also be used to place a stent and collect tissue samples.
As ERCP and PTC are more invasive procedures, there are some possible risks associated with these tests, including:
- allergic reactions to the sedatives or dyes used during the procedure
- injury to the gastrointestinal tract or bile ducts from the endoscope
- bruising and bleeding on the abdomen after PTC
- infection in the biliary system
- pancreatitis, or inflammation of the pancreas.
In some cases where a diagnosis is still uncertain after noninvasive and minimally invasive procedures, doctors may order a liver biopsy, where a thin needle is inserted through the abdomen and into the liver to collect a small liver sample for analysis. A biopsy can show abnormalities that are specific to forms of chronic cholangitis such as PBC and PSC or to other liver diseases. It also allows doctors to assess the extent and severity of liver damage, scarring, and inflammation.
Differential diagnosis of cholangitis
The symptoms of cholangitis can overlap with other diseases affecting the liver or the gastrointestinal system, including:
- hepatitis
- liver abscesses
- acute cholecystitis, or gallbladder inflammation
- pancreatitis
- perforated peptic ulcers, or holes in the stomach or upper part of the small intestine
- appendicitis, or inflammation of the appendix, a finger-shaped pouch that sticks out from the first part of the large intestine
- diverticulitis, where areas of the large intestine become inflamed or infected
- kidney infections.
Each of these conditions requires different treatment and management approaches, so it’s important to rule them out when diagnosing cholangitis. Doctors are usually able to do this through a series of blood and imaging tests, along with a thorough medical history and physical exam.
Challenges in diagnosing cholangitis
Because the symptoms of cholangitis can overlap substantially with several other conditions, it can be easily misdiagnosed. Many symptoms of cholangitis, especially those associated with chronic forms of the condition, can also be subtle and nonspecific.
If cholangitis or another liver disease is suspected, patients should seek advice from medical experts, such as hepatologists or gastroenterologists (specialists in liver or gastrointestinal diseases, respectively), who best understand how cholangitis is diagnosed. However, such experts — and the advanced imaging technology that’s sometimes required to diagnose cholangitis — may not be readily accessible in all regions, making it more difficult to diagnose.
Researchers are exploring new methods that may make it easier to diagnose cholangitis, particularly in regions with limited access to advanced technology. For example, some studies have tried to identify new biomarkers that could indicate the presence of PBC and PSC, and help distinguish these conditions from other liver diseases, via blood tests.
Liver Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- New animated video aims to support children living with biliary atresia
- New immune therapy for chronic hepatitis B slashes virus levels in trial
- Skipping PBC treatment leads to longer hospital stays, higher costs: Study
- Distinguishing between PFIC3, Wilson’s disease key for optimal outcomes
- The different ways fatty liver disease affects women vs. men
Related content