Steatotic liver disease diagnosis
Last updated Feb. 17, 2025, by Lindsey Shapiro, PhD

Diagnosing steatotic liver disease, a group of conditions marked by excessive fat buildup in the liver called steatosis, can involve a series of medical tests, including a physical exam, blood tests, imaging studies, and sometimes a liver biopsy.
SLD — known as fatty liver disease until a 2023 nomenclature update — is a common liver disease, but it usually does not cause symptoms early on. As a result, it is often found incidentally, when blood or imaging tests requested for other reasons show abnormal findings suggestive of SLD. If a person shows symptoms, a doctor may run additional tests to diagnose the disease, identify its underlying cause, and determine how far it has advanced.
Left untreated, SLD can result in serious issues such as cirrhosis, liver cancer, or liver failure that requires a liver transplant. Cirrhosis refers to liver scarring, or fibrosis, that is permanent and widespread, interfering with the organ’s function. The disease can also cause health problems that affect organs beyond the liver in the long term.
It is therefore critical to properly and promptly diagnose SLD. Doing so will allow patients to start treatment and implement lifestyle changes that can help slow, stop, and possibly reverse disease-related changes before they cause life-threatening complications.
Causes and risk factors
SLD can have a number of possible causes, including high alcohol consumption, pregnancy, or metabolic factors. It also can occur as a side effect of certain medications.
In the past, SLD was grouped into two main subtypes — alcoholic fatty liver disease and nonalcoholic fatty liver disease, then known as NAFLD — based on whether the disease was associated with excessive alcohol consumption.
Under the new nomenclature, alcoholic fatty liver disease is now referred to as alcohol-associated liver disease, or ALD. Most cases of NAFLD are now classified as metabolic dysfunction-associated steatotic liver disease, or MASLD, which is defined by the presence of cardiometabolic risk factors. The include being obese or overweight, having high blood sugar or type 2 diabetes, experiencing high blood pressure, or having high levels of fats such as cholesterol and triglycerides in the blood.
When MASLD progresses to cause liver inflammation and fibrosis, it’s called metabolic dysfunction-associated steatohepatitis, or MASH. This was formerly known as nonalcoholic steatohepatitis (NASH).
Signs and symptoms leading to diagnosis
At most stages, SLD is usually not accompanied by any obvious symptoms. If a person does have SLD symptoms, it’s often because the disease has progressed to more advanced stages, when liver function is starting to be affected.
Some of the earliest symptoms, which can be subtle and nonspecific, include:
- feelings of tiredness or fatigue
- malaise, or generally feeling unwell
- abdominal discomfort
- loss of appetite or nausea.
Symptoms that may indicate the disease has already progressed to cause more significant liver problems include:
- jaundice, or yellowing of the skin and whites of the eyes
- itchy skin, or pruritus
- small, spider-like blood vessels visible beneath the skin, called spider veins
- unexplained weight loss
- fluid buildup in the abdomen
- swelling in the legs, ankles, or feet
- redness of the palms of the hands
- dark urine
- pale stools
- easy bleeding or bruising
- altered mental status.
If a person is experiencing symptoms of SLD, regardless of whether these are mild and nonspecific or indicative of more significant liver damage, it is important to inform a doctor as soon as possible and get further tests to help diagnose the condition.
Initial steps for diagnosing SLD
In the presence of possible symptoms of SLD, a doctor will first collect a thorough medical history and conduct a physical exam.
For the medical history, the doctor will try to better understand which symptoms the person has been experiencing and for how long. The doctor will also ask questions regarding health conditions and lifestyle factors that could increase the risk of SLD, including:
- overweight or obesity
- type 2 diabetes
- high levels of cholesterol or triglycerides in the blood
- high blood pressure
- alcohol consumption
- prescribed and recreational medications
- low levels of physical activity
- diet with too many unhealthy foods and sugary drinks.
During the physical exam, the doctor will look for clinical signs of liver disease, such as:
- an enlarged liver
- jaundice
- fluid buildup in the abdomen.
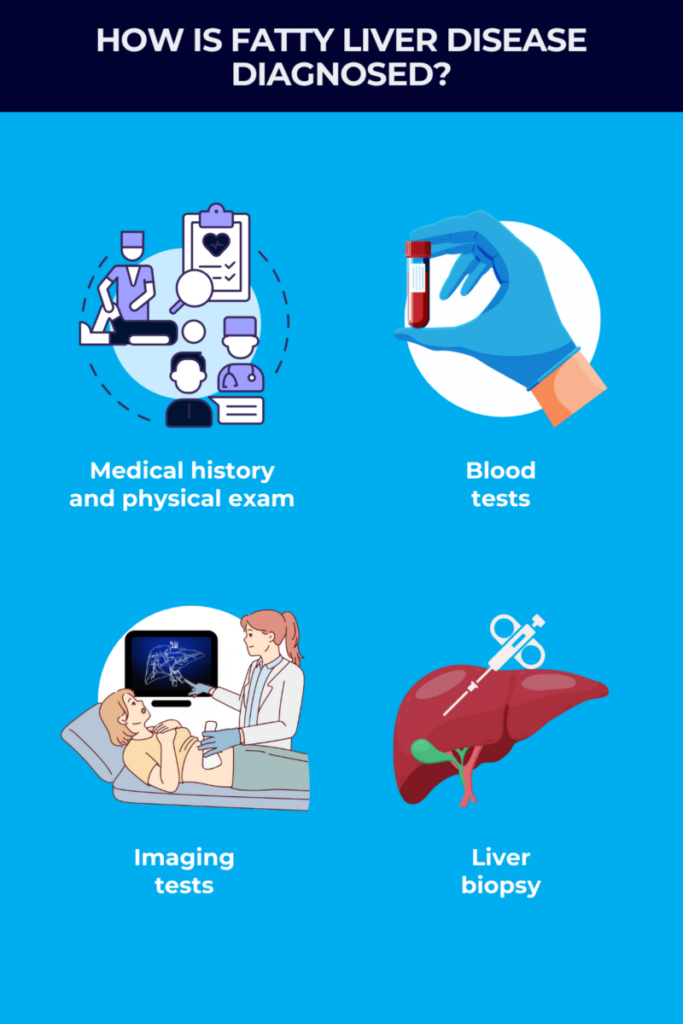
Diagnostic tools and procedures
If a doctor suspects SLD, a series of medical tests may establish a diagnosis, determine the disease stage, and/or rule out other diseases. Such tests may include:
- blood tests
- imaging tests
- liver biopsy.
Blood tests
Blood tests performed for other reasons can incidentally point toward a liver problem, prompting doctors to run more tests. For a person who is showing symptoms, these tests can help establish if there is indeed a problem with the liver, and if so, rule out other potential causes, such as viral hepatitis, or liver inflammation caused by a virus.
Testing can also offer information about the type of SLD by evaluating metabolic factors related to MASLD, like the levels of blood sugar (glucose) or cholesterol. Some things that might be checked for in SLD tests are levels of different enzymes or antibodies:
- Levels of liver enzymes, including alanine aminotransferase and aspartate aminotransferase, are usually higher than normal in people with SLD and often are checked via blood tests. These levels can be combined with those of other molecules commonly assessed in routine blood tests to calculate special scores of liver fibrosis, including the Fibrosis-4 index (FIB-4).
- Iron levels, which are often abnormal in people with liver diseases, may be checked with such testing.
- Levels of antibodies against hepatitis viruses, which can also cause liver problems, often are checked.
- Levels of glucose and markers of insulin resistance, typically elevated in type 2 diabetes, can be checked with testing.
- Cholesterol and triglyceride levels also can be tested. Higher-than-normal levels are a risk factor for MASLD.
Imaging studies
If blood tests are abnormal and suggest SLD, noninvasive imaging tests will usually be run to visualize the liver and identify the presence of steatosis. These tests may include:
- abdominal ultrasound
- CT scan
- MRI scan
- elastography.
The first-line imaging test for SLD is usually an abdominal ultrasound, which uses high-energy sound waves to create pictures of internal organs, including the liver, in the abdomen. This test can show signs of excess fat in the liver, as well as any indications of advanced liver fibrosis.
More advanced imaging tests, such as MRI or CT scans, might also be performed to get a better picture of what’s happening in the liver when an ultrasound doesn’t provide enough information. An MRI is considered more sensitive than an ultrasound at quantifying liver fat.
Elastography uses low-frequency vibrations during an ultrasound or MRI to measure the elasticity and stiffness of specific organs and tissues, with less elasticity and more stiffness reflecting a greater amount of scar tissue. A type of elastography called vibration-controlled transient elastography, which is usually performed using a device known as FibroScan, is also commonly used to assess liver fat and fibrosis. It uses a hand-held wand to produce ultrasound images.
Importantly, however, none of these imaging tests can definitively determine how far SLD has advanced.
Liver biopsy
A liver biopsy, which involves collecting a small sample of liver tissue and sending it to a lab for comprehensive analysis, is the only way to definitively distinguish MASLD from MASH, and to clearly determine how advanced a person’s SLD has become.
Because it’s a more invasive procedure than other tests, a liver biopsy will not always be used for a SLD diagnosis, although it may be needed in certain situations. A doctor may recommend one if a patient is believed to be at a high risk for advanced fibrosis or cirrhosis. In other cases, a doctor may recommend a liver biopsy to rule out other causes of liver disease and establish a SLD where other tests were unable to provide conclusive results.
There are a few ways a liver biopsy might be obtained. The most common is by inserting a thin needle through an incision in the abdomen and into the liver. The area where the needle is inserted will be numbed with a local anesthetic, so a person may feel pressure during the procedure, but it will not be painful. The procedure usually lasts 15 to 30 minutes.
While liver biopsy is safe when performed by an experienced physician, there are possible risks associated with such an invasive procedure, including:
- pain at the biopsy site
- internal bleeding
- infection
- accidental damage to nearby organs.
Differential diagnosis and other diagnostic challenges
A key challenge in diagnosing SLD is that a patient generally won’t have symptoms that prompt a doctor visit. The disease may not be caught until blood tests run for other reasons indicate abnormal liver function, or the person has symptoms associated with advanced disease.
Even when signs and symptoms of SLD are present, they can overlap with several other conditions that lead to fibrosis and cirrhosis. Some conditions that may be considered in an SLD differential diagnosis include:
- viral or alcohol-related hepatitis
- alpha-1 antitrypsin deficiency
- primary sclerosing cholangitis
- primary biliary cholangitis
- Wilson disease.
These other diseases need to be excluded before a SLD diagnosis can be established. In the presence of signs of SLD or other liver conditions, it is important to seek referrals to experts such as hepatologists, or liver specialists, who know what the signs of a steatosis are and how SLD is diagnosed.
Once steatosis is identified, major diagnostic challenges are determining if MASLD has progressed to MASH and establishing the degree of fibrosis. This is an important step when diagnosing SLD, as management approaches will look different depending on how advanced the disease is.
Because that information can’t be accurately determined with standard blood and imaging studies, a doctor will generally look at a person’s medical history, laboratory findings, and risk factors to determine who is most at risk of having advanced disease and may benefit from a liver biopsy.
What to do after a SLD diagnosis
Once a diagnosis is reached, a patient should start working with the healthcare team immediately to develop an appropriate plan for managing SLD and closely monitoring disease progression.
It will be important to understand the type and stage of disease, as the approach will differ depending on the underlying cause and how significantly the liver is affected.
For example, if a person has ALD, the doctor may recommend that the individual stop drinking alcohol. Someone with MALSD, meanwhile, may be advised to make lifestyle changes that help that person lose weight and reduce body fat.
Lifestyle modifications that can help maintain a healthy liver and stop or reverse liver damage include:
- eating a healthy diet
- exercising regularly
- avoiding alcohol and smoking
- managing stress
- getting enough sleep.
If MASLD progresses to MASH, liver damage may not be reversible and treatment may require more intensive interventions.
While it is important to start managing SLD as soon as possible, a patient should not make any lifestyle changes without talking to the healthcare team. Doctors can help the patient come up with a disease management and monitoring plan that makes the most sense in that person’s individual case.
Liver Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- New animated video aims to support children living with biliary atresia
- New immune therapy for chronic hepatitis B slashes virus levels in trial
- Skipping PBC treatment leads to longer hospital stays, higher costs: Study
- Distinguishing between PFIC3, Wilson’s disease key for optimal outcomes
- The different ways fatty liver disease affects women vs. men
Related content