GLP-1 agonists linked to lower risk of complications in MASLD, MASH
Such medications, used for weight loss, diabetes, include Ozempic, Wegovy
Written by |
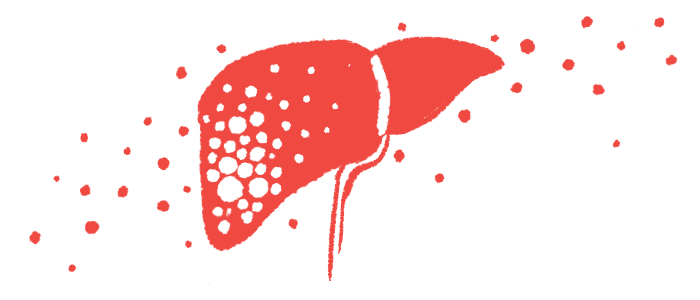
Use of glucagon-like peptide-1 (GLP-1) receptor agonists in people with metabolic dysfunction-associated steatotic liver disease (MASLD) or metabolic dysfunction-associated steatohepatitis (MASH) — forms of fatty liver disease — was associated with a reduced risk for major cardiovascular events, liver complications, and death, a study found.
GLP-1 receptor agonists, also simply called GLP-1 agonists, are an increasingly popular class of medications for weight loss and diabetes that include the well-recognized brand names Ozempic and Wegovy.
Specifically, the retrospective study found a “significantly lower risk of heart failure” as well as “all-cause mortality” after seven years, according to the researchers. Other benefits were seen for liver health.
“These findings highlight the potential of GLP-1 agonists in MASLD/MASH management, warranting further prospective studies,” the scientists. Prospective studies are those where people are followed over time to assess changes in outcomes.
The study, “Glucagon-like peptide-1 receptor agonists improve metabolic dysfunction-associated steatotic liver disease outcomes,” was published in the journal Scientific Reports.
Investigating possible benefits of GLP-1 agonists for MASLD, MASH
MASLD occurs when excess liver fat accumulates in people with cardiometabolic risk factors such as type 2 diabetes, also known as high blood sugar, and obesity. For some, it advances to a stage where liver fat gives way to inflammation and scarring, known as MASH, which can eventually lead to more serious liver damage and associated symptoms.
A key goal in treating MASLD is to control the cardiometabolic risk factors associated with it. Lifestyle changes such as diet and exercise can help prevent the disease from progressing, and in some cases, reverse it.
As such, scientists are investigating whether medications that induce weight loss might be of benefit for treating this common liver disease, which has also been “associated with significant cardiovascular [disease] and mortality,” the researchers wrote.
GLP-1 agonists work to control obesity and diabetes by mimicking the activity of GLP-1, a naturally occurring hormone that works in the gut and brain to regulate blood sugar and appetite.
Clinical trial data have shown the benefits of using these medications — such as reductions in liver fat and scarring — in people with MASLD or MASH. However, more research is needed to fully establish the long-term impact of such drugs on clinical outcomes in this patient group.
In this study, scientists affiliated with Thomas Jefferson University Hospital in Philadelphia investigated a possible association between the use of GLP-1 agonists and the prevention of major cardiovascular or portal hypertension events in adults with MASLD/MASH. Portal hypertension is a serious complication of liver disease characterized by an elevated pressure in the major vein that runs through the liver.
The researchers examined electronic health records of more than 12,000 adults with MASLD/MASH. Half had received a GLP-1 agonist after their diagnosis, with use documented at least twice, with at least three months in between. These patients were then matched across a range of demographic and clinical features with individuals who did not receive such medications and served as a control group.
Over a seven-year follow-up period, people who received GLP-1 agonists were significantly less likely to experience major cardiovascular events or portal hypertension events than those who did not, the data showed.
Specifically, after seven years, 3.4% of people given the medications had experienced heart failure, compared with 4.1% of those who did not. This amounted to a 28% lower risk with GLP-1 medications, per the researchers.
Findings show ‘potential clinical value’ of therapies to manage patient care
Other major cardiovascular events — such as a heart attack, chest pain due to reduced blood flow, or the need for procedures such as bypass surgery to restore normal blood flow — were experienced by 2.3% of the GLP-1 group and 3.3% of the control group after seven years. Here, the use of such medications was associated with a 41% lower risk among patients.
Likewise, the GLP-1 group was found to have a 54% lower risk of clinically significant events related to portal hypertension. Such events include fluid buildup in the abdomen, cirrhosis, or irreversible liver scarring, liver failure, and liver transplant. The data showed 1.2% of the GLP-1 group experienced such events after seven years compared with 2.3% of the control group.
The risk of these major clinical complications was similarly reduced at other evaluated timepoints, namely after one, three, and five years of follow-up.
GLP-1 agonists usage demonstrated a remarkable reduction in the risk of major adverse cardiovascular events, clinically significant portal hypertension events, new-onset heart failure, and overall mortality across all follow-up time points.
By the end of the follow-up period, 1.5% of people given GLP-1 medication and 4.2% of those not on these medications had died. GLP-1 medication use was associated with a significantly lower risk of death at all time points, lowering the risk by 77% at seven years.
“GLP-1 agonists usage demonstrated a remarkable reduction in the risk of major adverse cardiovascular events, clinically significant portal hypertension events, new-onset heart failure, and overall mortality across all follow-up time points,” the researchers wrote. “These outcomes underscore the potential clinical value of GLP-1 agonists in MASLD and MASH management.”
The scientists noted that due to some study limitations, including the research’s retrospective nature, further studies, following patients over time, will be needed to firmly establish how these medications affect major clinical events in people with MASLD or MASH.
The team also noted that another “intriguing avenue for future investigation” could be to evaluate the potential benefits of combining GLP-1 agonists with medications that work via different mechanisms.