Fatty liver disease overview: What you should know
Last updated March 15, 2024, by Marisa Wexler, MS

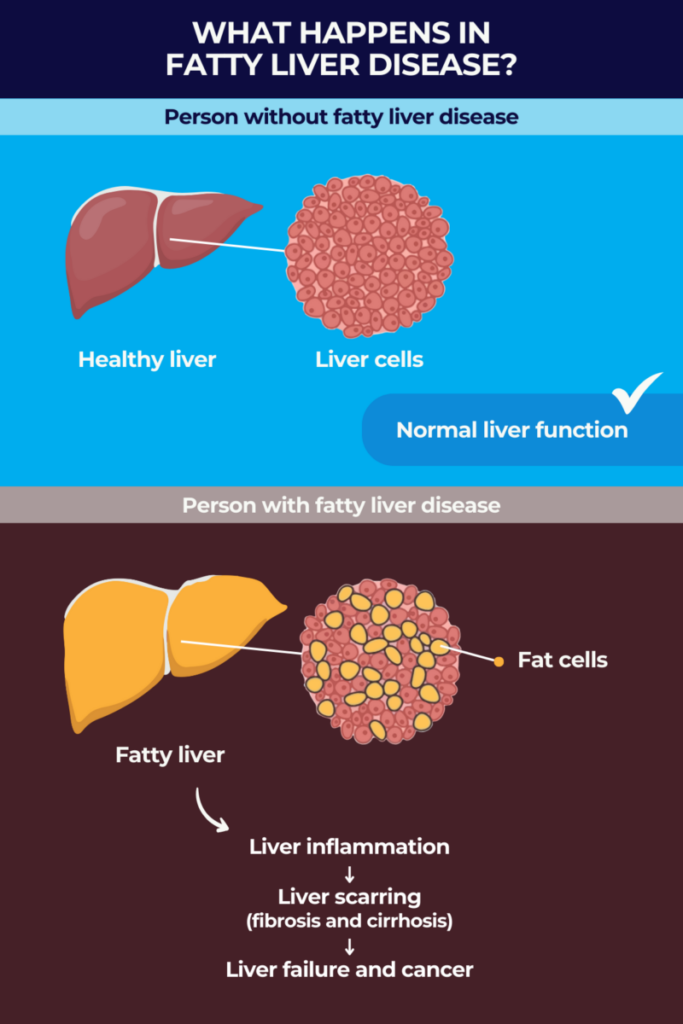
Fatty liver disease is a term used to refer to a group of disorders characterized by abnormal amounts of fat in the liver. Together, these diseases are estimated to affect more than one-third of people in the U.S. and other industrialized countries.
A healthy liver contains a small amount of fat, but when that percentage reaches 5% or more of the liver’s overall weight, it can start causing problems. Fatty liver disease often doesn’t cause noticeable symptoms at first, though it may result in fatigue, abdominal pain or other issues. In more advanced stages, however, the disease can lead to severe scarring of the liver and set the stage for liver cancer or liver failure.
Fatty liver disease is now more formally known as steatotic liver disease or SLD. The nomenclature, or the system of names used in a particular field, was updated in 2023 by an international group of liver societies and healthcare professionals. Their aim was to use a name more precisely descriptive — steatosis refers to the specific type of fat accumulation in liver cells that happens in fatty liver disease.
Types of fatty liver disease
Fatty liver disease has traditionally been divided into two main types — alcoholic or nonalcoholic — based on whether or not the accumulation of fat in the liver is associated with high alcohol consumption.
However, this nomenclature was changed in the 2023 update — to alcohol-associated liver disease (ALD) and metabolic dysfunction-associated steatotic liver disease (MASLD) — to more accurately reflect the real causes of the disease in each type. The new names also avoid terms such as “nonalcoholic” and “fatty,” which were deemed stigmatizing by most experts.
There also are fatty liver disease forms that can develop due to a combination of alcohol and metabolic factors, or as a side effect of medications, as well as forms associated with pregnancy.
Alcoholic fatty liver disease (AFLD)
The name alcoholic fatty liver disease (AFLD) has traditionally been used to refer to a form of the disorder that develops when liver damage occurs due to excessive intake of alcohol. This condition is now called alcohol-associated liver disease or alcoholic liver disease (ALD).
The liver normally can process small to moderate amounts of alcohol, but large amounts over the course of a long time period can lead to progressive damage. The first stage in alcohol-associated liver disease is steatosis, in which fatty deposits build up in the liver. This is followed by liver inflammation, known as alcoholic hepatitis, and irreversible scarring of liver tissue, called alcoholic cirrhosis.
Nonalcoholic fatty liver disease (NAFLD)
Nonalcoholic fatty liver disease (NAFLD), often simply called fatty liver disease, has traditionally been a catch-all term used to refer to any type of fatty liver disease that can’t be explained by excess alcohol intake.
Under the new nomenclature, most cases previously considered NAFLD are now classified as metabolic dysfunction-associated steatotic liver disease, or MASLD.
MASLD is defined by steatosis (fatty liver) in the presence of at least one of the following five cardiometabolic risk factors:
- high body mass index or waist circumference, indicating obesity or overweight
- high blood sugar or type 2 diabetes
- high blood pressure
- high triglycerides (a type of fat) in the blood
- high cholesterol in the blood.
In most people, NAFLD/MASLD does not cause any obvious problems — in fact, it’s estimated that nearly one-third of adults worldwide have this condition, and many are unaware of it.
But in some cases, MASLD can progress to cause liver inflammation and scarring, resulting in a more severe form of the disease that was previously called nonalcoholic steatohepatitis (NASH).
NASH, the fastest-rising cause of liver cancer worldwide, is now known as metabolic-associated steatohepatitis (MASH); in the U.S. it is estimated to affect about 5% of adults.
In addition to liver problems, people with NAFLD/MASLD are at increased risk of cardiovascular issues such as heart disease and stroke, and they also may be at higher risk of kidney disease.
Other chronic types of fatty liver disease
In the 2023 nomenclature update, experts also made a separate category, called metabolic dysfunction and alcohol-associated liver disease, or MetALD, to include people who meet diagnostic criteria for MASLD but also consume a high amount of alcohol.
Another disease type, called drug-related SLD, occurs as a side effect of certain medications, as well as some recreational drugs and industrial chemicals. There are dozens of substances that are known to induce steatosis, which include aspirin, certain chemotherapies and antibiotics, and cocaine.
There also are cases of fatty liver disease in which the person does not have a history of heavy alcohol use, exposure to other liver-injuring drugs, nor any cardiometabolic risk factors. Such cases where the cause cannot be determined are classified as cryptogenic SLD.
Acute fatty liver of pregnancy (AFLP)
Acute fatty liver of pregnancy (AFLP) is a rare form of fatty liver disease that develops during pregnancy — usually marked by symptoms that occur in the third trimester. Patients often first experience nausea, vomiting, reduced appetite, and abdominal pain, but AFLP can quickly progress to cause life-threatening liver damage.
This condition is estimated to affect as many as 1 of every 7,000 pregnancies. It’s thought to develop due to problems in processing fat molecules to provide the developing fetus with energy — but the causes of this type of fatty liver disease are poorly understood.
In most cases, AFLP resolves once the pregnancy is over, usually about seven to 10 days after delivery. Thus, management generally focuses on delivering the baby as quickly as possible while providing supportive care.
A liver transplant may be necessary in new mothers whose liver function doesn’t recover quickly after the pregnancy. Children born of a pregnancy affected by AFLP also should be monitored for signs of disorders that cause irregularities in fat processing.
The four stages and symptoms of fatty liver
The progression of fatty liver disease generally can be divided into four stages:
- Simple fatty liver, or steatosis, is the first stage, in which there are abnormal fat deposits in the liver, but no other notable symptoms or signs. As it can only be detected via medical tests, most people in this stage don’t know they have fatty liver disease.
- Steatohepatitis, the second stage, is marked by inflammation that damages the liver. This transition is what distinguishes MASLD from MASH, for example.
- Fibrosis, characterized by scar tissue starting to form in the liver, characterizes the third stage. This scarring can reduce the organ’s ability to function.
- Cirrhosis, the fourth and final stage, is marked by widespread and permanent scarring in the liver that substantially impairs liver function. This stage can occur years after the first signs of inflammation, and can lead to liver failure and liver cancer.
While some people in the early stages may experience fatigue, weakness, or abdominal pain, patients usually don’t have any obvious fatty liver symptoms. It’s only at more advanced stages of fatty liver that many patients experience more specific symptoms, which can include:
- nausea
- loss of appetite and weight loss
- itchy skin
- jaundice, or a yellow coloring of the skin and whites of the eyes
- swelling in the abdomen and/or limbs
- bleeding from the gastrointestinal tract.
Causes
In some forms of the disease, fatty liver causes are fairly straightforward. For example, alcohol-associated liver disease occurs because excess consumption of alcohol can cause metabolic changes that boost the production of fatty molecules in the liver while limiting their degradation. This results in the buildup of fatty deposits in the liver. Similarly, drug-related SLD is caused by the use of drugs or other substances that interfere with normal metabolism to cause steatosis.
Acute fatty liver of pregnancy is thought to develop because the pregnant person or the developing fetus are not processing fats properly. Meanwhile, MASLD is believed to be caused by an increase in the levels of fatty molecules or changes in how the body processes them.
The exact causes of pregnancy-related fatty liver disease and MASLD aren’t fully understood, although numerous risk factors have been identified.
Risk factors
The main risk factor for alcohol-associated liver disease is consuming alcohol heavily, especially for a prolonged period of time. Similarly, the use of certain medications or drugs is the main risk factor for developing drug-related SLD.
Other risk factors that increase the likelihood of developing fatty liver disease include:
- obesity or being overweight
- type 2 diabetes or insulin resistance
- high levels of triglycerides or abnormal levels of cholesterol in the blood
- metabolic syndrome, a condition defined by at least three of five traits, including a large waist size, high blood pressure, and high blood levels of triglycerides, cholesterol, and/or sugars
- polycystic ovary syndrome, known as PCOS
- obstructive sleep apnea
- low levels of thyroid, pituitary gland, and/or sex hormones
- older age, particularly an age older than 50
- smoking.
Diagnosis
The only test that can definitively diagnose fatty liver disease is a liver biopsy, in which a piece of the liver is surgically removed and taken to a laboratory for evaluation.
This test can conclusively identify signs of steatosis, as well as inflammation or scarring, so it also can be used to determine the stage of the patient’s fatty liver disease. However, because a liver biopsy is an invasive procedure, it often is not used for fatty liver diagnosis unless the patient shows notable signs of liver damage.
A range of other diagnostic tests may be used to help identify fatty liver disease:
- Blood tests can look for markers of liver damage. Results from blood tests also may be used to calculate biomarker scores that identify or rule out scarring in the liver.
- Imaging tests, such as ultrasound, MRI, or CT scans, may be used to image the liver. While these tests can’t reliably identify inflammation or scarring, they can detect signs of physical damage to the liver.
- Elastography, a newer type of imaging test, can determine how stiff the liver is. Because scar tissue is much stiffer than healthy tissue, this can help detect fibrosis.
Treatment
Fatty liver treatment generally consists of lifestyle changes aiming to limit further damage to the liver and to reduce the total amount of fat in the body. This can help manage existing disease and also help with fatty liver prevention.
Specific lifestyle changes that are commonly recommended for people with fatty liver disease include:
- abstaining from alcohol and other substances that can damage the liver
- dieting or changing eating habits to lose weight
- exercise.
Along with more exercise and better weight management, other fatty liver prevention measures can include improved stress management, getting appropriate sleep, and overall, maintaining better health.
People with NAFLD in particular, now known as MASLD, have metabolic alterations that put them at higher risk of developing cardiovascular diseases. Thus, it’s generally recommended that these patients lose about 3% to 5% of their total body weight to both reverse or control the liver disease and reduce their cardiovascular risk.
For people with more advanced disease (NASH or MASH), a gradual weight loss of 7% to 10% is recommended to reduce fat buildup in the liver. In some cases, medications or bariatric surgery may be considered along with lifestyle changes to help promote weight loss.
A medication called Rezdiffra (resmetirom) is also approved for use along with exercise and diet in some of these patients. In particular, the therapy has shown the ability to ease tissue scarring and reverse NASH in people with NASH and moderate to advanced liver fibrosis.
In alcohol-associated fatty liver disease, reducing alcohol intake — or, ideally, abstaining entirely — is the main method of treatment. Similarly, when another medication or drug is causing fatty liver, stopping exposure to the medication is the first line of treatment.
Across all types, management of fatty liver also involves getting treatment for other co-occurring conditions, especially metabolic issues such as diabetes that may worsen liver disease if not managed. Patients will usually require ongoing monitoring of liver health so that any issues can be addressed as soon as they arise.
In instances where liver damage becomes severe and irreversible, a liver transplant — a surgery in which a healthy liver from a donor is implanted to replace the failing organ — may be recommended.
Can fatty liver disease be reversed?
In some cases, with appropriate care and weight loss, the liver is able to heal itself, reducing inflammation, scarring, and steatosis. Reversing fatty liver disease generally is more feasible in the early stages of disease; if the disease progresses to cause cirrhosis, such damage is rarely reversible.
Diet
Eating a healthy diet is a critical part of managing fatty liver disease. While specifics will vary from person to person, the general dietary advice for people with fatty liver disease is to limit foods that are high in fats and sugars, while eating more fruits, vegetables, and whole grains, and giving preference to leaner meats.
Figuring out exactly what constitutes a healthy diet for any particular person requires a certain amount of individualization — and importantly, a fatty liver diet plan will only be helpful if the person is able to stick with it. It’s recommended that patients consult with an expert, such as a nutritionist, to design a diet plan that’s workable for them.
Regardless of exactly what foods a person is eating, limiting portion size also is a helpful way to promote weight loss. Further, given the link between fatty liver and alcohol, patients with any type of fatty liver disease should generally avoid alcoholic beverages of any type.
Life expectancy
Life expectancy for someone with fatty liver disease depends largely on the type of disease the individual has and how advanced it is when diagnosed.
For people with liver disease associated or not with alcohol, life expectancy is generally normal if the disease is caught early on — before extensive inflammation and tissue scarring are observed — and appropriate steps are employed to limit further damage.
If cirrhosis has already set in at the time of diagnosis, however, the disease is more likely to be life-limiting. When cirrhosis is caught early, life expectancy is about 10 to 15 years. But if the disease has already progressed to cause serious complications, such as bleeding or swelling in the abdomen, life expectancy is much shorter, at about three to five years.
Living well with fatty liver disease
Living with fatty liver disease involves making a number of lifestyle changes to manage and potentially reverse some of the liver damage that has accrued.
These include dietary changes and physical exercise to ensure patients lose weight in a healthy manner, as well as avoiding alcohol and cigarettes, and any other substances that can stress the liver.
It’s also important that patients receive all recommended vaccinations, particularly for hepatitis A and B. These liver infections are more likely to cause serious problems in people with preexisting liver disease.
Beyond managing the physical and health aspects, it’s also important to prioritize mental and emotional health. This may include stress management techniques including meditation or talk therapy. Patients also can seek out support groups and similar resources for comfort and solidarity, which can help in long-term management of the disease.
Liver Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Rare liver cancer found in toddler with Alagille syndrome
- Autoimmune hepatitis treatment zetomipzomib trial seeks patients
- Analyses on volixibat trial data in PSC, PBC slated for June
- Livmarli benefits seen across PFIC types, trial data show
- Our son’s Alagille diagnosis was our introduction to rare diseases
Related articles