PSC patients with IBD face higher risk of liver complications: Study
PSC-IBD combo represents 'unique' disease profile
Written by |
Primary sclerosing cholangitis (PSC) patients with inflammatory bowel disease (IBD) face a higher risk of liver-related complications and the need for a liver transplant than those without, according to a retrospective analysis of data from a U.S. clinical database.
The findings support the idea that PSC combined with IBD may represent a distinct and potentially more aggressive disease subtype, underscoring the importance of “careful monitoring of liver function in PSC-IBD patients,” the researchers wrote.
IBD is an umbrella term for diseases marked by gastrointestinal tract inflammation that often occur alongside PSC. The data showed that the risk of these liver-related outcomes was particularly higher for patients with ulcerative colitis, a subtype of IBD marked by colon and rectum inflammation.
The findings were described in the study, “Clinical Outcomes in Patients with Primary Sclerosing Cholangitis With and Without Inflammatory Bowel Disease,” published in Digestive Diseases and Sciences.
PSC is a rare, chronic liver disease that causes inflammation and scarring of the bile ducts — the tubes that carry the digestive fluid bile from the liver to the intestine. This damage can block bile flow, which, over time, can lead to irreversible liver scarring (cirrhosis), liver failure, and the need for a liver transplant.
‘Distinct’ disease course for PSC-IBD
Some 60% to 80% of people with PSC also have IBD, most often ulcerative colitis, and less commonly Crohn’s disease (a type that can affect any part of the gastrointestinal tract). When the two conditions co-occur, patients face a higher risk of gastrointestinal cancers, including bile duct cancer (cholangiocarcinoma) and colorectal cancer.
“PSC-IBD appears to represent a unique disease [profile] characterized by a distinct course of disease,” but “data are limited on liver disease progression in PSC-IBD,” the researchers wrote.
The two researchers at the Medical University of South Carolina retrospectively analyzed data from the TriNetX U.S Analytics Network Platform, which contains electronic medical records from more than 116 million patients.
Between January 2005 and June 2020, they identified 6,690 adults with PSC, of whom 3,678 (55%) also had IBD. These patients were less likely to be women (38% vs. 53%) and were diagnosed at a significantly younger age (mean age 43 vs. 54) than those with isolated PSC.
The PSC-IBD group was also significantly less likely to have cirrhosis at the time of diagnosis (18% vs. 24%) and more frequently treated with corticosteroids (strong anti-inflammatory medications), including prednisone (27% vs. 16%).
To ensure fair comparisons between the two groups, the researchers matched patients based on age, sex, and several laboratory and clinical characteristics. After matching, each group consisted of 1,714 people, and the two groups were similar in terms of liver disease severity and other health conditions.
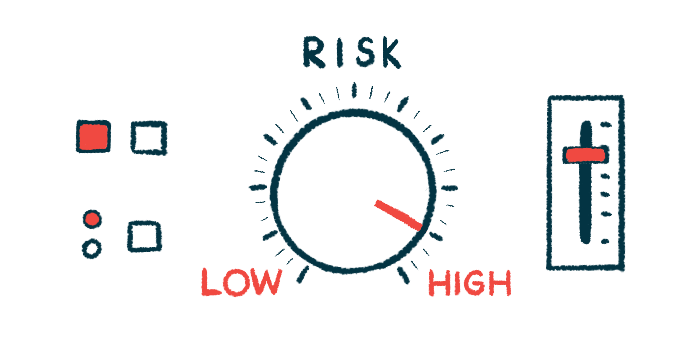
Over an average follow-up of five years, no significant differences in blood levels of liver damage markers were observed between groups. However, people with PSC-IBD were significantly more likely to experience liver-related complications.
The PSC-IBD group had a significantly higher cumulative rate of liver decompensation (cirrhosis that is so widespread that the organ can no longer work correctly) relative to the isolated PSC group (26.4% vs. 18.5%).
This reflected a 26% higher risk of liver decompensation events, including ascites (fluid buildup in the abdomen), variceal bleeding (bleeding from enlarged veins in the esophagus or stomach), and hepatic encephalopathy (brain dysfunction caused by toxin buildup when the liver cannot work correctly).
PSC-IBD patients were also significantly more likely to develop cholangiocarcinoma (9.6% vs. 6.3%), hepatocellular carcinoma (the most common type of liver cancer; 5.8% vs. 3.7%), and colorectal cancer (5.5% vs. 1.3%).
Having both PSC and IBD was significantly linked to a higher risk — by 50% — of needing and undergoing a liver transplant, but mortality rates were comparable between the PSC-IBD and isolated PSC groups (13.3% vs. 12.1%).
Further statistical analyses showed that cirrhosis at the study’s start more than doubled the risk of needing a liver transplant. Male sex and older age — particularly between 45 and 60 years — were also linked to higher transplant risk.
In terms of IBD subtypes, people with ulcerative colitis had significantly worse outcomes, showing significantly higher rates of liver decompensation events, liver transplant, cholangiocarcinoma, and colorectal cancer relative to people with isolated PSC. No such differences were observed for those with Crohn’s disease.
When the team looked only at participants with portal hypertension (increased pressure in the vein that carries blood to the liver) at the study’s start, they found that having both PSC and IBD continued to be linked to higher rates of liver decompensation events and liver transplant.
“Our analysis has shown an increased risk of liver-related complications, including an increased risk of portal hypertensive decompensating events and cholangiocarcinoma, and higher liver transplantation rates in PSC-IBD patients than in those with isolated PSC,” the researchers wrote. “These findings raise the possibility of [biological] interplay between IBD and PSC.”