TGF-beta Protein Fosters Conversion of Normal Liver Cells to Cancerous, Study Suggests
Written by |
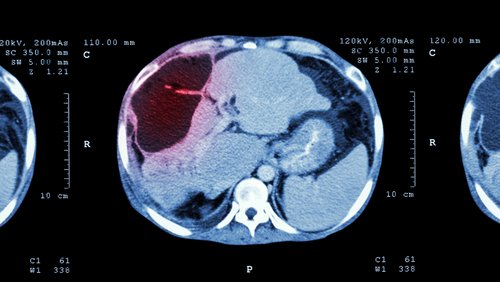
The transforming growth factor-beta (TGF-beta) protein promotes the conversion of normal liver cells to cancerous cells, a study indicates.
It also regulates liver cancer cells’ ability to migrate, the researchers said. Normal liver cells are known as hepatocytes, and the team studied their transformation into the most common type of liver cancer, hepatocellular carcinomas, or HCCs.
The study,“Transforming growth factor-β-induced plasticity causes a migratory stemness phenotype in hepatocellular carcinoma,” was published in Cancer Letters.
Researchers had previous examined “the relationship between the tumorigenic potential of TGF-beta and its ability to induce a process known as epithelial-mesenchymal transition, which favors the migration of cancer cells,” Isabel Fabregat, the senior author of the study, said in a press release. “The present work also shows that during that process, TGF-beta could also modulate the tumor cell’s ability to behave as a tumor initiator.”
TGF-beta is an important signaling protein that the body activates the response to cell damage. It turns on several signals as chronic liver diseases progress. Although it is involved in wound healing and repair of liver tissue, it can also trigger hepatocyte stress and cell death.
Researchers at the Bellvitge Biomedical Research Institute (IDIBELL), which is part of the IT-Liver European consortium, wanted to know if TGF-beta was an important player in two cell transformation processes. One was the hepatocyte transformation process. The other was the epithelial-mesenchymal transition (EMT) process, a mechanism that is essential to cancer progression.
TFG-beta plays a dual role in HCC, the team discovered. It can work as a tumor suppressor at the beginning of a malignant cell’s transformation. But it can also promote tumors in more advanced stages of the disease.
TGF-beta fostered what researchers called a partial EMT transition because HCC cells exhibited both epithelial and mesenchymal features. Epithelial cells have little capacity to migrate, so they usually stay at the tumor site. Mesenchymal-like cells can travel, however, so they are usually responsible for a tumor spreading to other areas of the body.
This mixed profile was associated with HCC cells developing an increased ability to migrate, transform, and become aggressive.
“Tumoral cells entering the circulatory or lymphatic system must have migratory capacity to be able to move and invade other body areas, but at the same time they must also acquire some stemness so that they can metastasize and expand once they have reached their destination,” Fabregat said.
TGF-beta levels in HCC patient samples correlated with the partial EMT profile, the team found.
“Curiously, the study shows that those cells with the greatest capacity as tumor initiators are not those of the mesenchymal type, but those that express an epithelial-mesenchyme intermediate phenotype, which would combine stemness with a greater migratory potential; this is the greatest innovation brought by our study,” Fabregat said.