Radiation-delivering Microspheres Fight Liver Cancer as Well as Chemo, Clinical Trial Indicates
Written by |
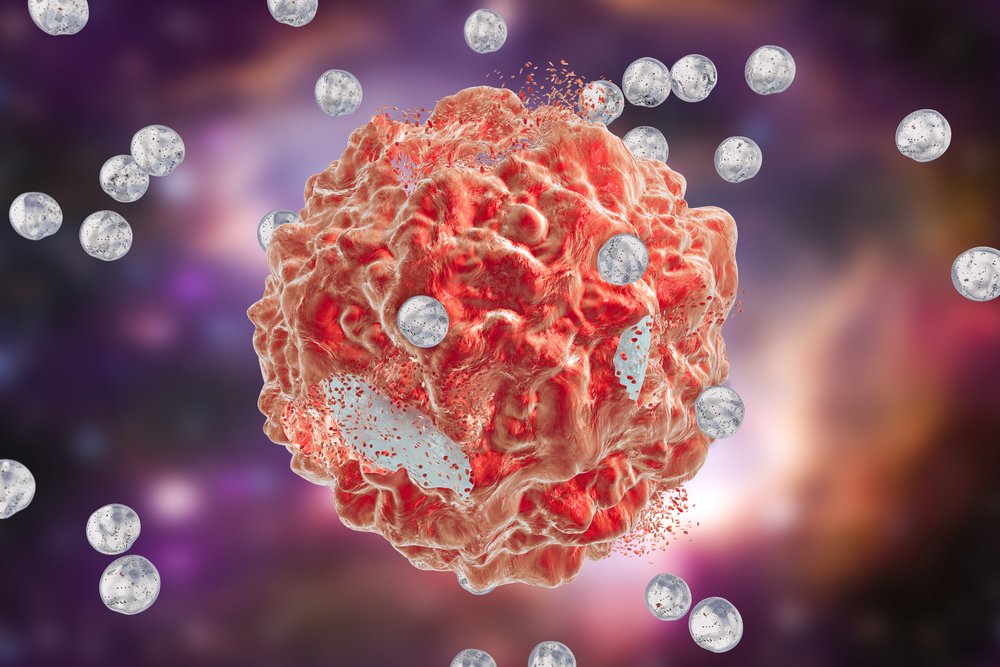
Radiation-delivering microspheres developed by Sirtex are as effective as Nexavar (sorafenib) chemotherapy against a liver cancer known as hepatocellular carcinoma (HCC), according to a Phase 3 clinical trial.
Sirtex’s SIR-Spheres Y-90 resin microspheres also generated fewer adverse side effects and gave patients a better quality of life, researchers said. Using the spheres to deliver radiation is called selective internal radiation therapy, or SIRT.
The SARAH trial covered people with advanced hepatocellular carcinoma and manifestations of the cancer that surgeons were unable to operate on.
“Neither sorafenib nor SIR-Spheres Y-90 resin microspheres produced a statistically significant difference in Overall Survival (OS) of the patients we studied,” Valérie Vilgrain, principal investigator of the SARAH study, said in a press release.
Researchers presented the trial’s findings at the International Liver Congress of the European Association for the Study of the Liver in Amsterdam. The presentation was titled “SARAH: a randomised controlled trial comparing efficacy and safety of selective internal radiation therapy (with yttrium-90 microspheres) and sorafenib in patients with locally advanced hepatocellular carcinoma.”
“In terms of what matters for patients, the findings from this first large head-to-head comparison of liver-directed STIR and systemic chemotherapy with sorafenib also show clearly that liver-directed procedures with SIR-Spheres result in a significantly better tolerance of treatment and quality of life,” Vilgrain added.
The SARAH study (NCT01482442), which started in December 2011, covered 459 patients. The goal was to see whether Sir-Spheres could perform as well or better than Nexavar in treating liver cancer.
Microspheres deliver high doses of radiation directly to tumors. SIR-Spheres deliver up to 40 times more radiation to liver tumors than conventional radiotherapy, while sparing surrounding healthy tissue, Sirtex said.
“For patients with advanced HCC or those failing TACE [chemotherapy infused directly into their livers], we have for the past 10 years relied upon oral systemic treatment with sorafenib, which was shown to extend survival compared to placebo, but also causes many side effects that can compromise patients’ quality of life,” Vilgrain said. “That is why we decided to see if treatment with a newer form of liver-directed therapy, selective internal radiotherapy, or SIRT, with SIR-Spheres could represent a better alternative.”
Patients treated with SIR-Spheres had the same median overall survival rate as those treated with Nexavar. But SIR-Spheres generated fewer and less severe side effects.
Ninety-four percent of patients treated with Nexavar had side effects, compared with 76 percent treated with SIR-Spheres. The most common adverse sides that patients reported, including infection, abdominal pain, nausea, vomiting, and fatigue, were more frequent and more severe in the Nexavar group, according to the study.
Researchers used a global health status questionnaire to evaluate patients’ quality of life after treatment. Those treated with SIR-Spheres reported that their quality of life was holding up, while those treated with Nexavar reported significant and sustained declines.
The results suggested that although SIR-Spheres and Nexavar are equally effective against liver tumors, the microspheres may be a better bet because they have no impact on patients’ quality of life.
“I believe this consideration should be a critical factor in selecting first-line treatment for this patient population in the future,” Vilgrain said.