Cholestasis overview: What you need to know
Last updated March 14, 2024, by Marisa Wexler, MS

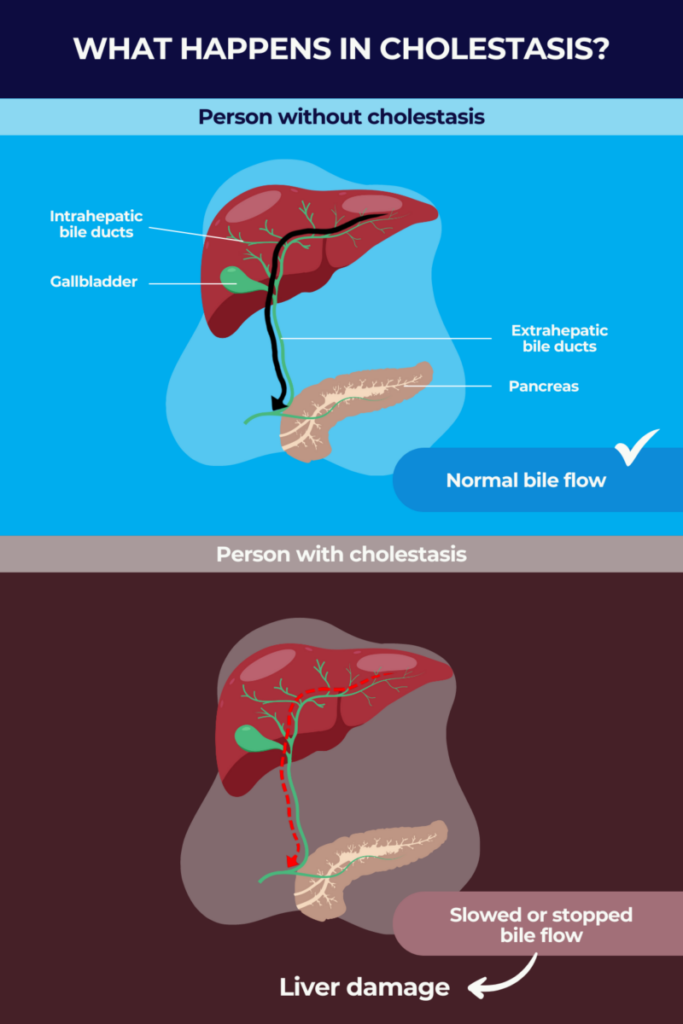
Cholestasis is a medical term used to describe a slowing or stalling of bile flow out of the liver. Bile is a yellow-greenish fluid produced by the liver that helps to break down certain fatty molecules and proteins into smaller pieces during digestion. It also carries certain waste products from the liver into the intestines to be excreted in feces.
Impaired bile flow can damage the liver and bile ducts and result in bile leakage into the bloodstream. That, in turn, can lead to digestive problems and symptoms such as jaundice, marked by a yellowing of the skin and the whites of the eyes, itching, and fatigue.
Cholestasis can occur as a complication of another liver disease or due to physical blockages in or near the liver; there’s also a specific form of cholestasis that can develop in the later stages of pregnancy. Identifying and addressing the underlying cause is key for managing cholestasis symptoms and preventing more serious liver health problems.
What is cholestasis?
Bile moves from the liver to the small intestine through a series of tubes called bile ducts. These ducts connect to the gallbladder, an organ under the liver where bile can be stored until it’s needed for digestion, and also to the pancreas, which makes enzymes needed for digestion. Together these organs and tubes make up the biliary system.
Cholestasis is a fairly general term that refers to any condition in which the flow of bile from the liver to the intestines is slowed or stopped entirely. The condition is classified as intrahepatic cholestasis when it occurs inside the liver — either due to problems in bile production or in the bile ducts — and as extrahepatic cholestasis when it affects bile flow outside the organ.
Among the causes of cholestasis can be blockages or abnormal narrowing, called strictures, in the bile ducts, which can occur due to high hormone levels in pregnancy, or as a complication of other chronic liver diseases. These diseases include biliary atresia, Alagille syndrome, and primary sclerosing cholangitis (PSC).
A few rare genetic diseases, collectively known as progressive familial intrahepatic cholestasis (PFIC), also can lead to cholestasis, most typically in early childhood. These are characterized by defects in bile formation or transport due to mutations in a number genes, each linked to a specific disease type.
Cholestasis affects people across all age groups, but children and adolescents may be more susceptible because the liver is still immature during these years. Women and men appear to be equally affected by the disease, but women are at a slightly higher risk of certain types of cholestasis.
Estimates as to how common is cholestasis depend on the disease type. For example, cholestasis of pregnancy, also known as intrahepatic cholestasis of pregnancy (ICP), is estimated to affect about 1-2 of every 1,000 pregnancies, while PFIC is believed to impact 1 in 50,000 to 10,000 people globally. Cholestasis in newborns, called neonatal cholestasis, affects about 1 in 2,500 live births.
Causes
There are several different potential cholestasis causes, which broadly can be divided into those that cause cholestasis inside or outside the liver. Causes of intrahepatic cholestasis include:
- intrahepatic biliary atresia
- Alagille syndrome
- primary biliary cholangitis (PBC)
- primary sclerosing cholangitis
- liver inflammation or hepatitis, including both acute and chronic forms
- alcoholic liver disease, a form of fatty liver disease
- progressive familial intrahepatic cholestasis
- hormonal effects on bile flow during pregnancy
- liver cancer or cancer that has spread to the organ
- serious bacterial infections that spread through the bloodstream, called sepsis
- getting nutrition exclusively through a vein.
Cholestasis may be experienced by people who are receiving nutrients exclusively and directly into the bloodstream, bypassing the digestive tract, because the intestines aren’t sending normal signals to the liver to prompt bile flow. That can result in bile buildup instead.
Some medications also may cause a form of intrahepatic cholestasis called drug-induced cholestasis. Among them are some antibiotics, such as penicillin, birth control pills and other medications containing hormones, and certain antipsychotics.
Extrahepatic cholestasis, for its part, can occur due to:
- certain cancers or tumors in the bile ducts and pancreas
- other nearby cancers that cause pressure on the bile ducts
- biliary strictures
- gallstones, or hardened bile deposits that form in the gallbladder and become stuck in bile ducts
- primary sclerosing cholangitis
- pancreas inflammation, known as pancreatitis.
Symptoms
The most common cholestasis symptoms include:
- jaundice
- dark-colored urine
- pale-colored stools
- itchy skin, known as pruritus.
The first three of these symptoms are related to bilirubin, a yellow-reddish waste product of red blood cell destruction that is incorporated with bile in the liver and eliminated in stool and urine.
A reduction in bile flow can lead to the leakage of its components into the bloodstream. An excess of bilirubin in the skin results in jaundice. Meanwhile, increased bilirubin excretion by the kidneys leads to dark-colored urine, and reduced excretion through the intestine causes light-colored stools.
Itching also is believed to be related to the accumulation of bile products in the skin. Moreover, prolonged cholestasis-related jaundice can lead to the formation of fatty yellow deposits, called xanthomas, in the skin.
The reduced levels of bile getting into the intestines also can cause issues in digesting and absorbing fatty molecules and fat-soluble vitamins — such as vitamins A, D, E, and K — which can lead to nutritional deficiencies.
Depending on the underlying cause, some people with cholestasis also may experience additional symptoms such as:
- fatigue
- fever
- loss of appetite
- nausea and vomiting
- pain in the upper right part of the abdomen.
Intrahepatic cholestasis of pregnancy
Intrahepatic cholestasis of pregnancy (ICP) is a form of cholestasis that develops during pregnancy. The most common pregnancy-related liver disease, ICP typically appears late in the second trimester or early in the third trimester, when hormone levels are at their highest. Some cases, though, have developed as early as five weeks of gestation.
The condition is thought to develop due to a combination of genetic and environmental factors, and high levels of reproductive hormones that can reduce bile flow, particularly estrogen, during later stages of pregnancy. Though the exact causes aren’t fully understood, a few risk factors that increase the likelihood of having ICP have been identified, including:
- a South American or North European descent
- personal or family history of ICP
- a co-occurring chronic liver disease
- pregnancy involving more than one fetus, such as twins, triplets, etc.
- pregnancy at an older age, such as 35 or older
- pregnancy during winter.
Usually the most noticeable symptom of IPC is itchy skin. Other symptoms of cholestasis of pregnancy can include jaundice, nausea, vomiting, or low appetite, as well as pale stools, dark urine, and upper right abdominal pain.
While ICP usually resolves on its own after pregnancy ends, it can increase the risk of major health problems for both the mother and the developing fetus.
Treatment typically involves ursodeoxycholic acid (UDCA), a cholestasis medication that can help promote the movement of bile through the bile ducts, as well as supportive care to relieve symptoms and keep the mother and the fetus healthy. In some cases, healthcare providers may also recommend the baby be delivered early, at around 37 weeks of gestation.
Diagnosis
A number of tests may be used to help confirm a cholestasis diagnosis:
- A physical examination and detailed medical history can be used to look for symptoms and signs of cholestasis, and to identify any risk factors.
- Blood tests may be used to look for signs of liver damage and/or bilirubin, as well as other bile components in the blood.
- Imaging tests, such as an abdominal ultrasound, MRI, or CT scan, can help to visualize the structure of the biliary system and identify blockages or areas of damage.
- A liver biopsy, where a small piece of the liver is surgically removed and taken to a lab for study, may be used to confirm intrahepatic cholestasis.
- Endoscopic retrograde cholangiopancreatography (ERCP) can be used to visualize the bile ducts, and is a minimally-invasive procedure in which an endoscope, or a thin, flexible tube with a tiny camera on the end, is inserted through the mouth into the digestive tract. ERCP also may be used to help address some cholestasis causes, such as removing bile duct blockages.
Treatment
The overall goal of cholestasis treatment is to restore bile flow, ease symptoms, and manage any cholestasis complications or other underlying health problems. An early cholestasis diagnosis and prompt treatment often can help to prevent the condition from progressing to cause more serious liver problems.
Treatment for cholestasis will generally vary based on its underlying cause and severity, and often will vary from person to person. If a medication is suspected to be the cause, stopping or replacing it for a similar one may ease the symptoms of cholestasis. Similarly, if an infection is the likely cause, treatment with antibiotics or antivirals may help ease or resolve the condition. But other forms of the disease may be more difficult to treat.
Other cholestasis treatment options may include:
- cholestasis medications such as UDCA (sold as Urso and Actigall) and cholestyramine (sold as Prevalite and Locholest, among others) to help reduce bile buildup and/or relieve symptoms like itching
- surgical or endoscopic procedures to remove blockages in cases caused by bile duct obstruction
- lifestyle changes such as dietary modifications to ensure proper nutrition, as well as avoiding alcohol and other substances that can stress the liver.
For PFIC in particular, two oral medications — Bylvay (odevixibat) and Livmarli (maralixibat) — are approved in the U.S. for reducing pruritus, or itching, in children and adults.
Living with cholestasis
People living with cholestasis usually need to go to regular medical checkups so they and their healthcare team can monitor their liver function and address any health issues that arise. Depending on the type of cholestasis, some patients will be able to stop regular monitoring once cholestasis is resolved, whereas others might require lifelong monitoring.
Because cholestasis limits a person’s ability to break down and absorb fatty molecules and fat-soluble vitamins, dietary changes may be recommended to ensure patients get enough nutrition.
In particular, following a low-fat diet can help relieve symptoms that occur when fat isn’t digested properly. Patients may receive supplements of certain fats that can be easily digested without bile, as well as any vitamins found at deficient levels.
High-fiber diets also help maintain a healthy liver function, and people with any form of liver disease are generally advised to avoid alcohol and other substances that may put stress on the liver. Avoiding such substances may prevent additional liver damage and also may aid in the prevention of cholestasis.
Getting regular physical exercise also is an important part of maintaining overall health for most people with cholestasis.
In addition, some patients may experience itching relief by applying moisturizing and cooling agents to the skin or showering with cold water. Adjusting clothing items to avoid skin irritation and friction also can help to provide some relief.
Living with cholestasis can be stressful and may take a toll on a person’s mental health. Apart from steps to manage the disease itself, it’s also important to prioritize caring for oneself and getting support where needed. Support groups are available online for some specific types of cholestasis, including ICP and PFIC. More general organizations such as the Childhood Liver Disease Research Network, known as ChiLDReN, or the American Liver Foundation also may provide support for people affected by cholestasis.
Liver Disease News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Abnormal amino acid profile seen in biliary atresia infants after birth
- Our daughter’s PFIC diagnosis made us rethink drinking at Christmas
- Hepatitis D treatment combo granted new designations in US, EU
- Committee recommends seladelpar approval in EU for treating PBC
- Diet rich in omega-3 fatty acids may lower risk of ICP, scientists say
Related articles